Gynecologist vs. OBGYN: Roles, Education, and Career Insights
- A gynecologist specializes in women’s reproductive health outside of pregnancy.
- An OB-GYN is trained in both gynecology and obstetrics, covering reproductive care and pregnancy.
- The main difference between these professionals is that OB-GYNs handle childbirth and pregnancy, while gynecologists focus solely on non-pregnancy reproductive care.
One of the oldest recorded references to women’s health is the Kahun Gynaecological Papyrus. This manuscript dates back to ancient Egypt and contains 34 detailed paragraphs that address medical issues specific to women. It’s proof that interest in this area of care stretches back thousands of years. Yet even today, despite its long-standing importance, conversations about women’s health, especially regarding the reproductive system, can still feel shrouded in discomfort or taboo.
This reluctance often leaves gaps in understanding, even on fundamental topics. For instance, many people struggle to distinguish between a gynecologist vs. obgyn, unsure where their roles differ and where they overlap.
✅ Request information on AUA's MD program TODAY!
What Is a Gynecologist?
A gynecologist is a medical professional who specializes in the female reproductive system. These physicians focus specifically on the reproductive system’s organs, functions, as well as overall health throughout a woman’s life.
A gynecologist’s expertise covers areas many are familiar with, such as menstrual cycles, hormonal changes, reproductive health concerns, and fertility. Naturally, this makes them a central figure in routine reproductive care.
What Is an OB-GYN?
An OB-GYN is a physician who is trained in both obstetrics and gynecology. Their expertise combines reproductive care with pregnancy and childbirth expertise.
Like gynecologists, they handle general reproductive health, but they also provide care throughout pregnancy, labor, delivery, and even support recovery after birth. This dual focus makes the role of OB-GYNs much broader and enables them to guide patients through a broader range of reproductive and maternal health needs.
Gynecologist vs. OB-GYN: Key Differences
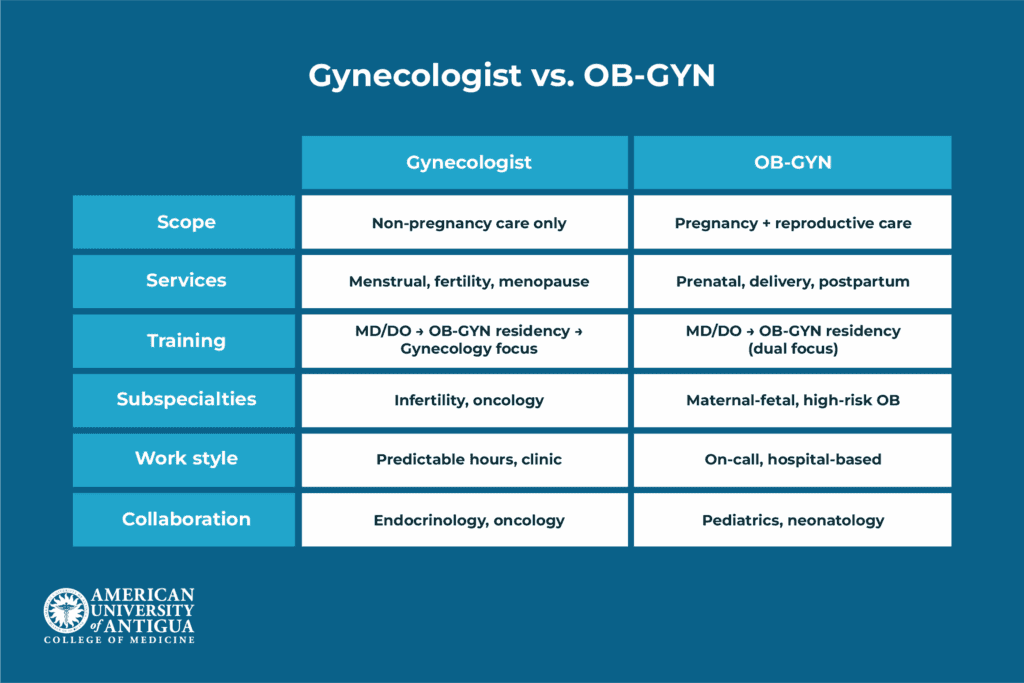
It’s clear that both roles deal with female reproductive health, which is why people often use the terms interchangeably. However, to understand how they differ, it helps to look at what each professional specifically handles in their practice, the education that prepares them for these roles, their career outlook, and what other specialists they tend to collaborate with.
Services offered
Both gynecologists and OB-GYNs provide routine reproductive care such as pelvic exams, Pap smears, contraception counseling, and screening for infections. But, beyond these overlapping responsibilities, their scopes diverge.
Gynecologists focus entirely on reproductive health outside of pregnancy. They address a wide range of concerns, including menstrual irregularities, fertility issues, menopause management, as well as conditions such as endometriosis and polycystic ovary syndrome (PCOS). Preventive care is another component of their role, encompassing sexual health education, screenings for infections, and hormone therapy to manage symptoms associated with hormonal imbalances or aging.
OB-GYNs, on the other hand, combine all the services of a gynecologist with the added expertise of obstetrics. Their training equips them to oversee prenatal care, monitor fetal development, and guide patients through labor and delivery. They are also responsible for addressing complications during pregnancy, managing high-risk pregnancies, and providing postpartum care to ensure recovery and maternal well-being after childbirth.
Education and training
The course of study for both gynecologists and OB-GYNs, as is the case with most other physician types, begins along the same path before branching into distinct areas of focus. It starts with an undergraduate degree, usually in a pre-medical track or a science-related field such as biology or chemistry. This stage provides the foundational coursework needed to meet medical school prerequisites and prepare for the Medical College Admission Test (MCAT).
Following this, aspiring physicians enter medical school to earn either a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree. Medical school typically spans four years: the first two focus on classroom-based study of core subjects such as anatomy, physiology, pharmacology, and pathology, while the final two years involve hands-on clinical rotations. These rotations expose students to various specialties, including internal medicine, surgery, pediatrics, and women’s health, helping them build practical skills and decide on their area of interest.
After graduating from medical school, both future gynecologists and OB-GYNs begin a four-year residency in obstetrics and gynecology. During residency, they train extensively across both fields. This includes managing labor and delivery, performing gynecologic surgeries, diagnosing and treating reproductive health conditions, and providing preventive care. Residency is highly immersive, combining clinical practice with surgical training and exposure to both routine and complex cases, ensuring that all physicians in this track develop a comprehensive understanding of women’s health.
From here, the pathways diverge. Physicians who choose to focus solely on gynecology enter practice dedicated exclusively to reproductive health outside of pregnancy. Those who remain as OB-GYNs continue with dual training, maintaining both their gynecologic and obstetric responsibilities to care for patients throughout all phases of reproductive health and pregnancy.
Further specialization is also an option through fellowship programs. Gynecologists may pursue subspecialties such as reproductive endocrinology and infertility, minimally invasive gynecologic surgery, or gynecologic oncology. OB-GYNs, on the other hand, often subspecialize in areas tied more closely to pregnancy and maternal care, including maternal-fetal medicine or urogynecology. These additional fellowships typically last two to three years and allow physicians to develop expertise in highly focused fields, expanding their career opportunities and the scope of care they provide.
Career opportunities and demand
OB-GYNs generally have broader employment options since their training covers both pregnancy-related and non-pregnancy reproductive care. Because of this, OB-FYNs are able to work in labor and delivery units, maternal-fetal medicine, and comprehensive women’s health settings, in addition to standard gynecological roles.
Gynecologists often have more predictable work hours since they do not manage childbirth or respond to emergency obstetric cases. Whereas OB-GYNs, on the other hand, frequently take on-call shifts to attend births and handle pregnancy complications, which can make their schedules more demanding. While both fields offer opportunities in specialized surgery and academic positions, OB-GYNs typically have greater access to hospital-based careers tied to obstetrics and high-risk pregnancy care.
When it comes to job outlook, data for these roles is typically grouped together. Employment in this category has remained relatively steady since 2019, with vacancies increasing by about 1.5% nationwide during that time. Demand is expected to rise modestly, with projections indicating approximately 1,200 new jobs by 2029. This stability reflects a steady need across both obstetric and gynecological care, making either path a viable option for those entering the field.
Collaboration with other specialists
Gynecologists and OB-GYNs both work within multidisciplinary teams, but the specialists they collaborate with most often reflect their different areas of focus.
Gynecologists frequently coordinate with reproductive endocrinologists for fertility evaluations and hormone-related care, as well as oncologists in managing gynecologic cancers like cervical or ovarian cancer. They also work closely with urologists on pelvic floor or urinary health issues, and with primary care physicians to integrate reproductive health into broader wellness plans. Their collaborations are centered on long-term reproductive care and preventive health.
OB-GYNs, while also engaging in these areas, extend their collaborative network into pregnancy and maternal care. They routinely partner with pediatricians, maternal-fetal medicine specialists for high-risk pregnancies, neonatologists for newborn care in complicated deliveries, and anesthesiologists during labor and surgical procedures such as cesarean sections. Their teamwork is focused on ensuring safe pregnancies, deliveries, and postpartum care, in addition to ongoing reproductive health.
This distinction means that while both roles intersect with similar fields, gynecologists tend to collaborate more on chronic and preventive reproductive issues, whereas OB-GYNs work in settings that require coordination around childbirth and acute maternal care.
Pros and Cons of Each Career Path
From all we’ve established thus far about both career options, it’s clear that they are both strong choices. However, weighing the pros and cons of each career path is helpful when deciding between the two, particularly because their roles overlap in many areas.
Gynecology career
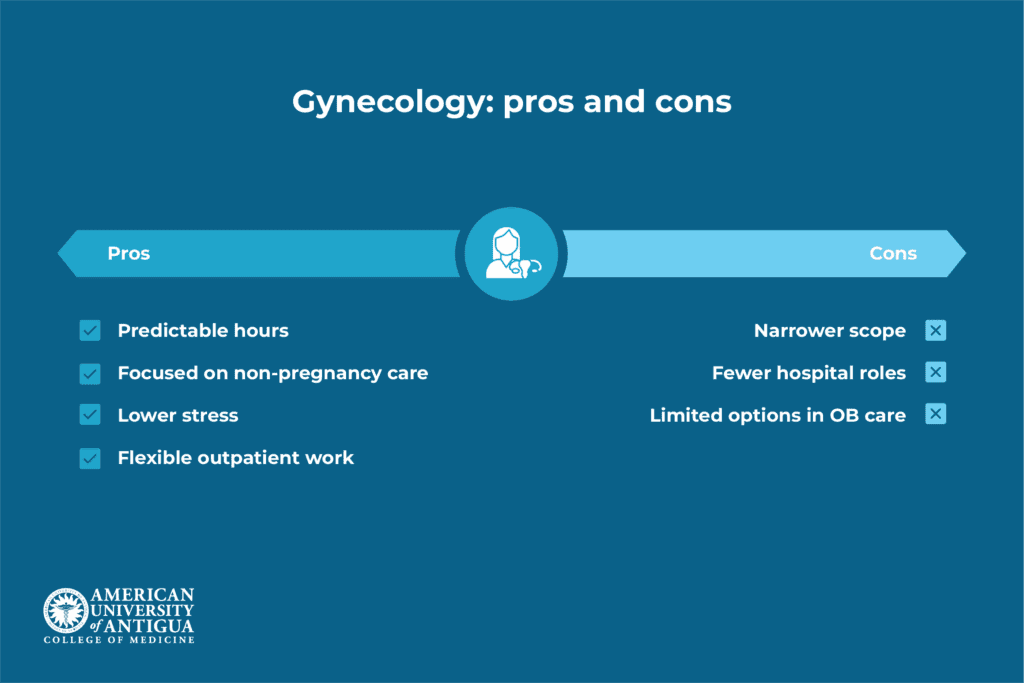
When looking at gynecology as a standalone specialty, there are several notable benefits to consider, such as:
- More predictable work hours without on-call labor and delivery responsibilities
- Focused expertise in non-pregnancy reproductive health, menopause, hormonal issues, and gynecologic surgery
- Lower stress compared to emergency obstetric scenarios or unpredictable birth schedules
- Greater flexibility for outpatient or private practice settings
At the same time, there are limitations that come with choosing a gynecology-only path:
- Narrower employment scope due to the exclusion of obstetrics and childbirth care
- Limited opportunities in hospital labor and delivery units or high-risk pregnancy care
- Fewer options in comprehensive women’s health settings where obstetric training is valued
OB-GYN career
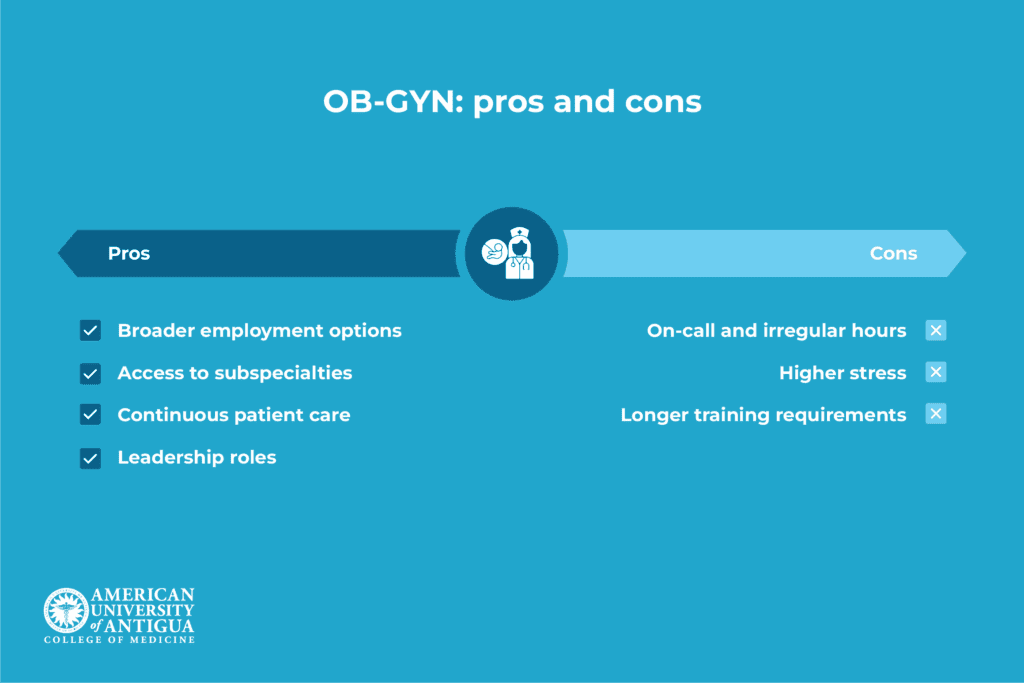
For those who pursue combined training in obstetrics and gynecology, the career offers the following advantages:
- Broader employment opportunities, combining both obstetric and gynecologic care
- Access to specialized fields like maternal-fetal medicine and high-risk pregnancy management
- Greater involvement in hospital-based roles and leadership positions in women’s health departments
- Ability to provide continuous care from pregnancy through long-term reproductive health
However, the OB-GYN route also comes with its own set of challenges, including:
- Unpredictable hours with on-call shifts and emergency obstetric cases
- Higher stress linked to managing labor, delivery, and urgent pregnancy complications
- Longer residency and training demands compared to non-obstetric gynecology
Choose the Right Fit for Your Future
Deciding between gynecology and OB-GYN ultimately depends on your preferred work-life balance, clinical interests, and long-term goals. Some are drawn to the stability and consistency that come with a narrower focus, while others prefer a role that offers a broader range of responsibilities and a faster pace.
Neither path is inherently better than the other. Therefore, taking time to consider what matters most to you, from your ideal schedule to the kind of day-to-day work you enjoy, will help you make a choice that feels both practical and fulfilling.
The Bottom Line
Gynecologists and OB-GYNs, in addition to diagnosing and treating, also advocate for women’s health. So, if you are drawn to medicine and want to be part of a specialty where your work directly impacts lives, focusing on women’s health is a path worth considering.
Training as a gynecologist or OB-GYN begins with a strong medical education, and AUAMED’s MD program provides the foundation you need to take that first step. Through our curriculum and supportive learning environment, you’ll gain the skills and experience essential to pursuing these careers.
Women’s health deserves nothing less than dedicated professionals committed to advancing it, and your career could be part of that change.
Frequently Asked Questions (FAQs)
Can you see an OB-GYN if you are not pregnant?
You can see an OB-GYN even if you are not pregnant, as they provide both obstetric and gynecologic care throughout different stages of a woman’s life.
Are most gynecologists also obstetricians?
Technically, a lot of gynecologists are trained and certified to handle both women’s reproductive health and pregnancy-related care. Therefore, in that sense, they are also obstetricians.
What is the role of an OB-GYN during labor?
During labor, an OB-GYN monitors the mother and baby, manages delivery, and addresses any complications to ensure a safe birth.
Is being a gynecologist or OB-GYN doctor worth it?
Being a gynecologist or OB-GYN can be worth it for those passionate about women’s health. Both options offer fulfilling medical careers with growing demand.
✅ Request information on AUA's MD program TODAY!