Types of Patients in Healthcare: Understand Their Needs
Key Takeaways
- Understanding different patient types helps healthcare professionals provide personalized and effective care.
- Communication should vary by patient type – emergency patients require quick instructions, while those with chronic conditions need more detailed explanations.
- Recognizing patient needs allows healthcare professionals to manage time and resources efficiently.
- Healthcare professionals can better adapt to diverse patient needs by staying informed, respecting cultural differences, and using technology to enhance care.
In healthcare, one size does not fit all. Patients have diverse backgrounds, conditions, and needs that shape how they experience treatment and care. Understanding the different types of patients is essential for healthcare professionals to provide effective, personalized care.
Whether addressing the urgency of an emergency case or providing ongoing support for a chronic condition, recognizing these differences directly impacts treatment planning, communication, and care delivery. By identifying the specific needs of each patient, providers can improve outcomes, build stronger patient relationships, and allocate healthcare resources more efficiently.
✅ Request information on AUA's MD program TODAY!
YOUR PATH TO SUCCESS BEGINS HERE
Different Types of Patients
Patients can be grouped in several ways, and each category can influence how healthcare professionals provide care. Recognizing these differences helps ensure that treatment is both personalized and effective.
In this section, we’ll explore five main aspects that help define different patient types: their current status in the healthcare system, the level and kind of care they require, the medical conditions they have, their behavior and attitude toward treatment, and their social and demographic background. Let’s take a closer look at each one.
Patient status
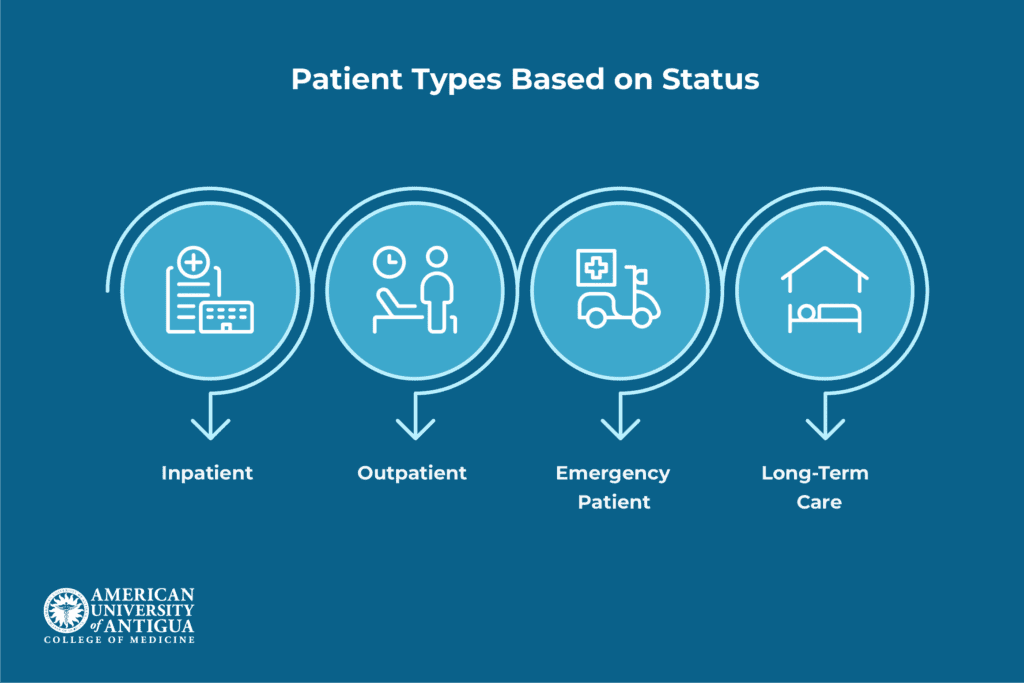
Patient status refers to where a person is within the healthcare system and how urgent their care needs are. Common types of patients based on status include:
- Inpatients: Stay in the hospital and are treated by hospital doctors, surgeons, or specialists.
- Outpatients: Visit clinics or doctor’s offices for check-ups, tests, or treatments and are usually seen by primary care physicians or specialists.
- Emergency patients: Go to the emergency room and are treated by emergency doctors who must act quickly due to time-sensitive conditions.
- Long-term care patients: May live in nursing homes or receive ongoing care at home, often supervised by geriatricians or rehabilitation specialists.
Communication depends on the patient’s status. Emergency doctors typically give brief, clear instructions because time is critical. In contrast, long-term care providers may engage in longer discussions with patients and families to plan ongoing treatment.
The type of care also depends on status. For example, emergency patients might need immediate surgery, while outpatients may only need a prescription or routine evaluation.
Patient needs
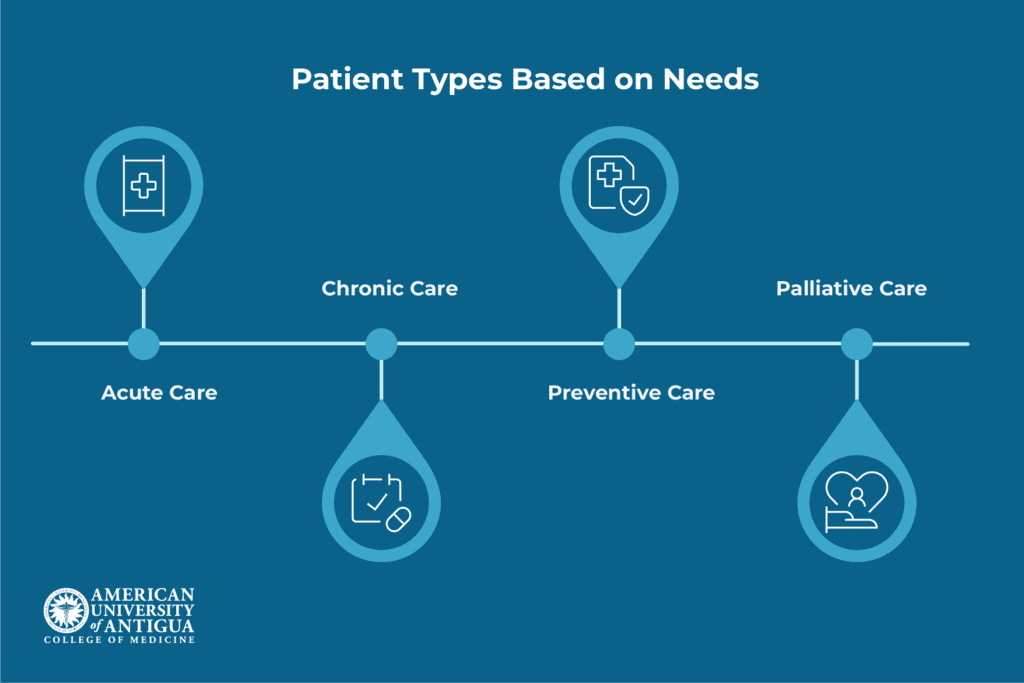
This category focuses on what kind of care a patient needs and how much support they require. Based on this, patients may need:
- Acute care: Patients have sudden or serious health problems and are usually treated by emergency or hospital doctors.
- Chronic care: Patients have long-term conditions like asthma or high blood pressure, which are often managed by internists or specialists.
- Preventive care: Patients are mostly healthy and visit family doctors for regular check-ups and screenings to stay well.
- Palliative care: Patients with serious illnesses are supported by doctors who focus on comfort, especially near the end of life.
Communication varies based on the patient’s needs. Chronic care patients benefit from ongoing education and regular updates to manage their condition. Palliative care patients and their families require compassionate, honest, and supportive conversations.
Treatment is also different for each type. Acute care patients may need immediate procedures or medications. Chronic care patients need long-term care plans, including lifestyle guidance and daily medications. Palliative care patients often prioritize pain relief, emotional support, and dignity rather than curative treatment.
Medical conditions
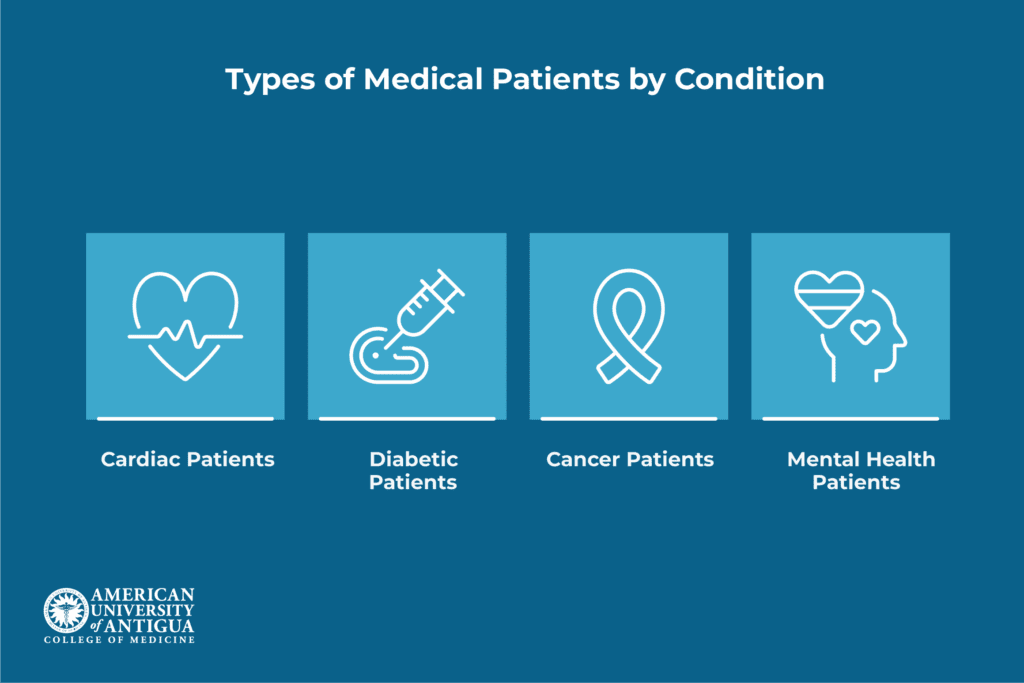
Patients are often grouped by the specific health problem or condition they have. Examples of these patient types include:
- Cardiac patients: Treated by heart specialists called cardiologists
- Diabetic patients: Managed by endocrinologists who help control blood sugar levels and diet
- Cancer patients: Treated by oncologists who develop treatment plans involving chemotherapy, radiation, or surgery
- Mental health patients: Cared for by psychiatrists, therapists, or psychologists, depending on the condition
Communication also depends on the medical condition. For example, cancer patients need detailed information about treatment options, side effects, and prognosis. Meanwhile, mental health patients may need more time to build trust and feel comfortable to share their thoughts and emotions.
Treatment also depends on the condition. A cardiac patient may need diagnostic tests and medications to control blood pressure or heart rhythm. A diabetic patient might need insulin, blood sugar monitoring, dietary planning, and regular check-ups. Mental health care could involve talk therapy, medication, crisis intervention, and support groups.
Behavior and attitude
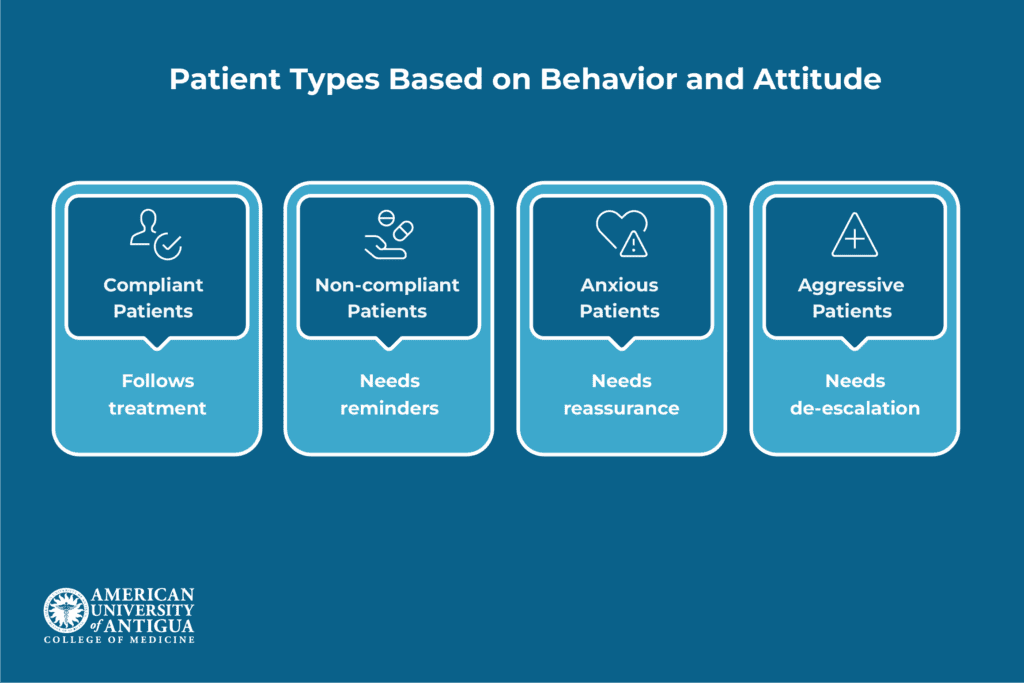
A patient’s behavior and attitude can affect how well they follow treatment and how doctors approach their care. Common types include:
- Compliant patients: Follow their doctor’s advice and are usually easy to manage
- Non-compliant patients: May skip medication or appointments, often requiring additional support from care teams or social workers
- Anxious patients: Feel nervous or fearful about treatment and benefit from gentle care and reassurance
- Aggressive patients: May act out or be confrontational, often needing intervention from mental health professionals or specialized care teams
Communication strategies differ based on behavior. Anxious patients may need calm, step-by-step explanations. Non-compliant patients respond better to motivational strategies and simplified instructions. Aggressive patients require a safe, structured environment and calm, professional communication.
Care delivery also adapts accordingly. A non-compliant patient with high blood pressure might need frequent follow-ups and simplified care routines. An anxious patient with chest pain may need extra time and emotional support before tests or procedures.
Demographics and social factors
A person’s age, culture, language, income, and living situation can all affect how they receive care and how doctors interact with them. Patient types in this group include:
- Pediatric patients: Children treated by pediatricians
- Elderly patients: Cared for by geriatricians who specialize in age-related conditions
- Low-income patients: Often see family doctors or public health workers who help them access affordable care and resources
- Non-English-speaking patients: May be treated by any doctor but often need interpreters or translated materials
- Culturally diverse patients: May have beliefs, customs, or expectations that influence how they view health and treatment
Doctors must adjust their communication methods accordingly. This can include using simple language, visual aids, translation services, or culturally sensitive explanations. Showing respect and building trust are essential to effective care.
Care also adapts to these factors. A low-income patient might need help accessing low-cost medications or transportation. An elderly patient might require mobility support, help managing multiple medications, or reminders for follow-up care. A non-English-speaking patient may need extra time during appointments to ensure understanding and informed decision-making.
Benefits of Understanding Patient Types
Understanding the different types of patients and adjusting treatment accordingly is an important part of delivering high-quality care. Key benefits include:
- Improved patient outcomes: Faster recovery, fewer complications, and improved management of chronic conditions.
- Enhanced communication: Ensuring clear and appropriate communication, which builds trust and helps patients follow their treatment plans.
- Better resource management: Allocating time, staff, and equipment more efficiently, reducing waste and avoiding unnecessary delays.
- Reduced provider burnout: Making tasks more predictable and manageable, which reduces stress for healthcare workers and increases job satisfaction.
- Personalized care delivery: Developing care plans that align with the patient’s health status, background, and lifestyle, making treatment more relevant and effective.
How Healthcare Professionals Can Adapt to Each Patient Type
Adjusting your medical approach to align with patient types not only builds trust but also leads to better health outcomes and greater efficiency. Here are several strategies healthcare professionals can use:
- Training and education: Continuous learning ensures providers stay current with the best practices for managing a wide range of patient types. Medical schools like the American University of Antigua (AUA) offer comprehensive training that includes clinical rotations and exposure to diverse patient populations, helping students build both knowledge and confidence.
- Cultural competence: Understanding a patient’s cultural background, including beliefs, customs, and health practices, can greatly improve the provider-patient relationship. This helps reduce misunderstandings and ensures care is respectful and appropriate.
- Flexibility in communication and care: Different patients respond to care in different ways. Some may need more detailed explanations, while others may prefer quick, clear instructions. Adjusting tone, language, and communication style helps meet each patient where they are, improving cooperation and satisfaction.
- Use of patient-centered technologies: Digital tools like translation services, electronic health records, and telehealth platforms enhance care delivery, particularly for patients with language barriers or chronic conditions. These technologies streamline communication and provide better continuity of care.
- Interdisciplinary teamwork: Collaborating with professionals from other fields, such as social work, physical therapy, or mental health, ensures patients receive well-rounded support. This is especially important for those with complex or long-term needs.
Conclusion
Recognizing and adapting to different types of patients is essential for ensuring high-quality care that meets individual needs. By understanding patient status, needs, behavior, and background, healthcare professionals can improve communication, optimize resource use, and enhance overall patient satisfaction.
For those interested in further developing their skills in this area, AUA offers comprehensive training that prepares future healthcare providers to care effectively for diverse patient populations. Apply now to begin your medical career and make a lasting impact in healthcare.
Frequently Asked Questions
Which types of patients are measured in length?
Pediatric patients are often measured in length, especially infants and toddlers.
What are the most common health conditions seen in healthcare?
Common health conditions seen in healthcare include heart disease, diabetes, respiratory infections, hypertension, and mental health disorders.
✅ Request information on AUA's MD program TODAY!