Rheumatologist vs Endocrinologist: Roles, Training, Careers
Key Takeaways:
- Rheumatologists treat joint and autoimmune diseases, while endocrinologists focus on hormone-related issues like diabetes and thyroid problems.
- Despite having different specializations—rheumatology for musculoskeletal issues and endocrinology for hormones—both specialties require medical school, residency, and a fellowship.
- Both professions deal with long-term ailments, and they may collaborate when conditions overlap, such as when diabetes affects joints or arthritis has an impact on hormones.
- Both specialties are in high demand due to more people needing care, leading to more job opportunities and higher salaries.
Autoimmune diseases happen when the body’s immune system attacks its own healthy cells, affecting different organs and systems. These diseases can cause pain, inflammation, and long-term damage to joints, muscles, bones, and other parts of the body.
✅ Request information on AUA's MD program TODAY!
YOUR PATH TO SUCCESS BEGINS HERE
Rheumatologists and endocrinologists are two types of doctors who treat these conditions, but they focus on different areas. Rheumatologists mostly treat joint and musculoskeletal problems, while endocrinologists focus on hormone-related issues.
In this article, we will look at the roles, training, and career paths of both rheumatologists and endocrinologists, comparing the similarities and differences between these two specialties.
What Is a Rheumatologist?
Rheumatologists are medical professionals who specialize in treating rheumatic conditions, which include diseases that affect the joints, muscles, bones, and immune system. These diseases often cause symptoms such as pain, swelling, stiffness, and inflammation.
Their job includes:
- Examining patients
- Ordering tests
- Diagnosing conditions
- Creating treatment plans, which may include medications, therapy, and lifestyle changes
People typically visit a rheumatologist when they have ongoing joint pain, swelling, fatigue, or signs of autoimmune diseases that don’t get better with general treatments. In return, rheumatologists help patients manage their conditions, prevent them from getting worse, and improve their overall quality of life.
What Is an Endocrinologist?
An endocrinologist is a doctor who focuses on treating problems related to hormones and the glands that produce them. Hormones are a crucial element of our body function as they help control key body functions like metabolism, growth, and mood.
Their job includes diagnosing hormone imbalances, running tests, and creating treatment plans, which may include medications and lifestyle changes.
People usually see an endocrinologist when they have symptoms like unexplained weight changes, tiredness, thirst, or trouble with their metabolism. Endocrinologists help manage these problems and keep hormone levels balanced, improving the patient’s health.
Rheumatologist vs Endocrinologist: Key Differences
As we established above, rheumatologists and endocrinologists are both doctors who deal with distinct medical conditions.
But their differences don’t lie only in the health issues they treat. Below we will explain in detail the main differences between rheumatologists and endocrinologists, including areas of specialization, education and training, patient communication, and career and salary outlook.
Autoimmune conditions
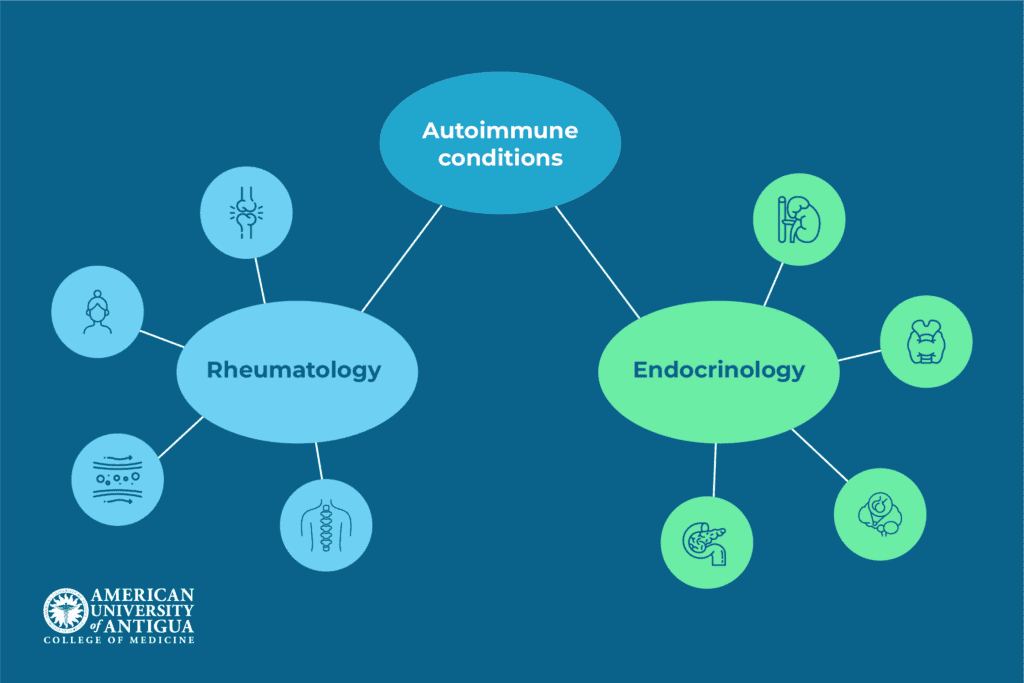
Both doctors treat autoimmune conditions however, they differ on the type of autoimmune health issues they treat. Below we will list the main autoimmune diseases and disorders each doctor treats.
Rheumatology
The rheumatologist’s role is to treat autoimmune conditions such as:
- Rheumatoid Arthritis (RA): This condition typically affects the hands and feet and is characterized by pain, swelling, and stiffness in the joints caused by an immune system attack. It can weaken the joints over time and make movement difficult.
- Systemic Lupus Erythematosus (SLE): This is a disorder in which the immune system attacks various body parts, such as the skin, kidneys, heart, and lungs. It may result in minor or severe flare-ups of symptoms, such as fatigue, joint pain, and rashes.
- Psoriatic Arthritis: This condition can develop in people who have psoriasis, a skin condition. It results in red, scaly skin areas as well as stiffness, edema, and joint pain, especially in the fingers and toes.
- Ankylosing Spondylitis: This type of arthritis affects the spine and pelvis, causing pain and stiffness. The spine may eventually fuse together, reducing the range of motion. It can also have an impact on other joints.
- Vasculitis: This condition is characterized by inflammation of the blood vessels, which can harm tissues and organs. If left untreated, it can cause major issues like blood clots and organ failure.
- Scleroderma: This condition causes the skin and connective tissues to thicken and tighten, which can make movement difficult. Its effects on internal organs, such as the lungs and heart, can cause major health problems.
Endocrinology
On the other side, endocrinologists treat hormone-related autoimmune conditions such as:
- Type 1 Diabetes: This condition happens when the immune system mistakenly targets the beta cells in the pancreas. This leads to a low level of insulin production, a hormone that is crucial for regulating blood sugar levels. The high levels of sugar in the body can cause a variety of health issues that can lead to serious complications if unmanaged.
- Hashimoto’s Thyroiditis: This disorder occurs when the immune system attacks the thyroid gland, making it less active. This causes symptoms including depression, weight gain, and fatigue since the thyroid controls metabolism and energy.
- Graves’ Disease: It’s characterized by an overactive thyroid due to immune system stimulation. This results in symptoms including anxiety, an elevated pulse, and weight loss.
- Addison’s Disease: In Addison’s disease, the immune system attacks the adrenal glands, which produce important hormones. This results in symptoms including low blood pressure, fatigue, and weight loss.
- Autoimmune Hypophysitis: This rare condition causes inflammation of the pituitary gland, which controls hormone production. It can cause symptoms like tiredness, headaches, and problems with vision, and may need hormone replacement treatment.
Education and training
While both follow a similar educational pathway to becoming a doctor, there are some key differences that differentiate rheumatologists from endocrinologists. Let’s explore their med-school journey,
Rheumatologist
Becoming a rheumatologist requires completing a bachelor’s degree, usually in a science-related field, followed by four years of medical school. After medical school, rheumatologists must complete a 3-year residency in internal medicine, where they gain broad medical knowledge and experience.
After that, they pursue a 2-3 year rheumatology fellowship, where doctors concentrate on autoimmune diseases and musculoskeletal conditions. During this time, they take courses in immunology, pharmacology, and musculoskeletal diseases, while also gaining hands-on experience in diagnosing and treating patients.
Moreover, rheumatologists can advance their careers by engaging in research, attending professional conferences, and obtaining further certifications or subspecialties, such as pediatric rheumatology.
Endocrinologist
A similar path leads to becoming an endocrinologist, but the emphasis is on the endocrine system, which regulates hormones in the body. Following four years of medical school and earning a bachelor’s degree, endocrinologists begin a three-year internal medicine residency.
After that, students finish a two to three-year fellowship in endocrinology, where they research diseases, including diabetes, thyroid problems, and metabolic disorders that are related to hormones. The fellowship combines practical patient care with instruction in hormone function, metabolism, and reproductive health.
Endocrinologists can further their careers by doing research, earning further certifications, and participating in endocrinology-focused conferences.
Communication with patients
Chronic health conditions require distinct care and communication due to their ongoing nature. Thus, rheumatologists and endocrinologists play a key role in addressing symptoms while also assisting their patients with the care and ongoing guidance they need.
Rheumatologists
Rheumatologists communicate with patients by focusing on joint pain, inflammation, and managing long-term conditions like arthritis or lupus. They discuss how to control symptoms, follow treatment plans, and take medications to avoid flare-ups and further damage.
Since many of their patients live with chronic pain and disability, rheumatologists also pay attention to the emotional side of care, listening to concerns about quality of life. They work closely with patients to track progress and adjust treatments to meet their needs.
Endocrinologists
As endocrinologists focus on conditions involving hormones, their meetings with patients often center on discussing how to manage the patient’s condition, such as preventing complications or lowering blood sugar levels.
Throughout their regular visits with patients, endocrinologists consider lifestyle factors, including exercise and diet, and emphasize the need to follow treatment recommendations.
In addition, endocrinologists monitor hormone levels, adjust medication as needed, and offer emotional support to their patients because some hormone-related diseases may lead to chronic health issues.
Career and salary outlook
Being a doctor means you will have a lucrative career (which reflects the long period of studying) with guaranteed job prospects, as people will always be in need of doctors. And, as autoimmune diseases are on the rise, both rheumatologists and endocrinologists are seeing increased opportunities.
Rheumatologist
According to a study conducted by the Association of American Medical Colleges (AAMC), during the 2021-2036 period, there will be a shortage in various specialties, including rheumatology. The shortage is projected to result from a slow supply of physicians. The demand for specialist doctors is on the rise as the US population continues to age, and the number of autoimmune diseases continues to rise.
In the future, the demand for rheumatologists will likely keep growing, leading to more job opportunities in hospitals, private practices, and academic roles.
As for salary, rheumatologists have seen steady increases due to the growing need for their expertise. Their pay can vary based on location, experience, and work setting, but as of 2024, rheumatologists earn between $203,231 to $326,072, with most professionals earning an average of $258,710 annually.
Endocrinologist
Endocrinologists have also seen a growing demand for their services, and as hormone-related issues such as diabetes are on the rise, this is expected to continue in the coming years.
With the rise of such autoimmune conditions, more endocrinologists are needed to diagnose and treat these diseases. This, in turn, will increase the demand for endocrinologists, creating more job opportunities.
Salary-wise, endocrinologists have experienced steady growth as well. Their pay depends on factors like experience, location, and work environment. However, as of 2024, endocrinologists earn between $197,382 and $343,149, with an average annual salary of $261,000.
Similarities Between Rheumatology and Endocrinology
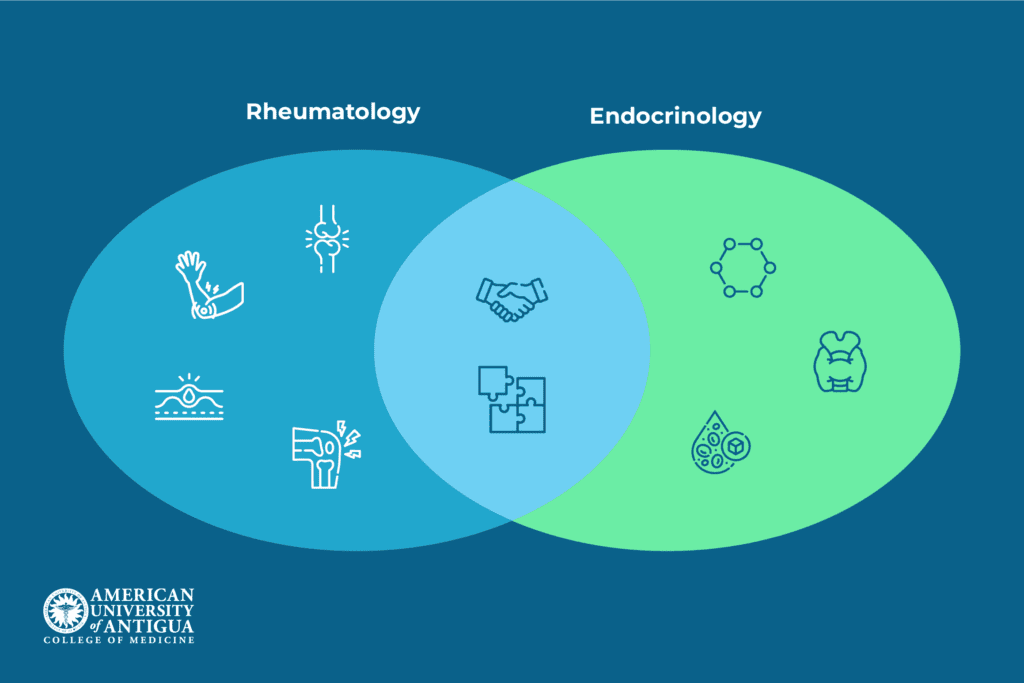
Though rheumatology and endocrinology are different fields, they have some similarities. Both deal with chronic conditions that need long-term care and can affect a person’s daily life. Patients in both specialties often require ongoing treatment, lifestyle changes, and education to manage their conditions.
There are also times when these two fields overlap. For example, rheumatoid arthritis can cause hormonal issues, and diabetes can lead to joint problems like a frozen shoulder. In these situations, rheumatologists and endocrinologists collaborate to treat both issues. Through this collaboration, they can create a complete treatment plan that addresses all aspects of the patient’s health.
Which One Should You Choose?

When deciding between rheumatology and endocrinology, you should think about your interests, skills, and future career goals. Both specialties are rewarding, but they focus on different health issues.
So, based on which aspect of medicine sparks your interest more, you can decide if rheumatology or endocrinology might be a better fit.
It’s also important to consider where you want to work. Do you envision yourself working in a hospital, research setting, or teaching setting? An answer to this question can illuminate the decision you will take for your future career.
Another practice you can take before deciding is to shadow doctors in both fields, talk to mentors, and get some hands-on experience.
Conclusion
In conclusion, rheumatologists and endocrinologists play key roles in treating chronic and autoimmune diseases, but they focus on different areas.
Both fields offer rewarding careers, and the choice between them should depend on your personal interests and career goals. Consider what excites you most and choose the path that best fits your skills and aspirations.
Curious about a medical career? Check out AUAMED’s programs today!
Frequently Asked Questions
Which organs of the body would be treated by an endocrinologist?
An endocrinologist treats organs like the thyroid, pancreas, adrenal glands, and pituitary gland.
Who is the best doctor for autoimmune diseases?
The best doctor for autoimmune diseases is a rheumatologist.
What is the most common disease treated by an endocrinologist?
The most common disease treated by an endocrinologist is diabetes.
✅ Request information on AUA's MD program TODAY!