Stages of Anesthesia: From Induction to Recovery
Key Takeaways
- Anesthesia is the use of drugs to block pain and awareness, allowing patients to safely undergo medical procedures and surgeries.
- The four stages of anesthesia, first described by Dr. Arthur Guedel in the early 20th century, outline the patient’s progression from induction to surgical anesthesia.
- The stages include induction (Stage 1), excitement (Stage 2), surgical anesthesia (Stage 3), and overdose (Stage 4), each with distinct characteristics and clinical significance.
- Stage 4 is unsafe, which is why modern anesthesiologists carefully monitor patients to prevent them from ever reaching this point.
So much of modern medicine, and especially surgery, would be impossible without anesthesia. It allows patients to undergo procedures without pain, while giving doctors the ability to work safely and effectively.
Anesthesia itself refers to the use of drugs to block sensation and awareness, and it is managed by a dedicated field of medicine known as anesthesiology. Physicians who specialize in this field, anesthesiologists, carry the responsibility of ensuring patients remain stable and comfortable throughout surgery.
✅ Request information on AUA's MD program TODAY!
One of the most important areas they must master is understanding the stages of anesthesia. These stages describe how a patient’s body and consciousness change as anesthesia takes effect. Recognizing them is crucial because it allows anesthesiologists to carefully guide patients into the right depth of anesthesia, maintain stability during the procedure, and bring them safely back to consciousness afterward.
What Are the Stages of Anesthesia?
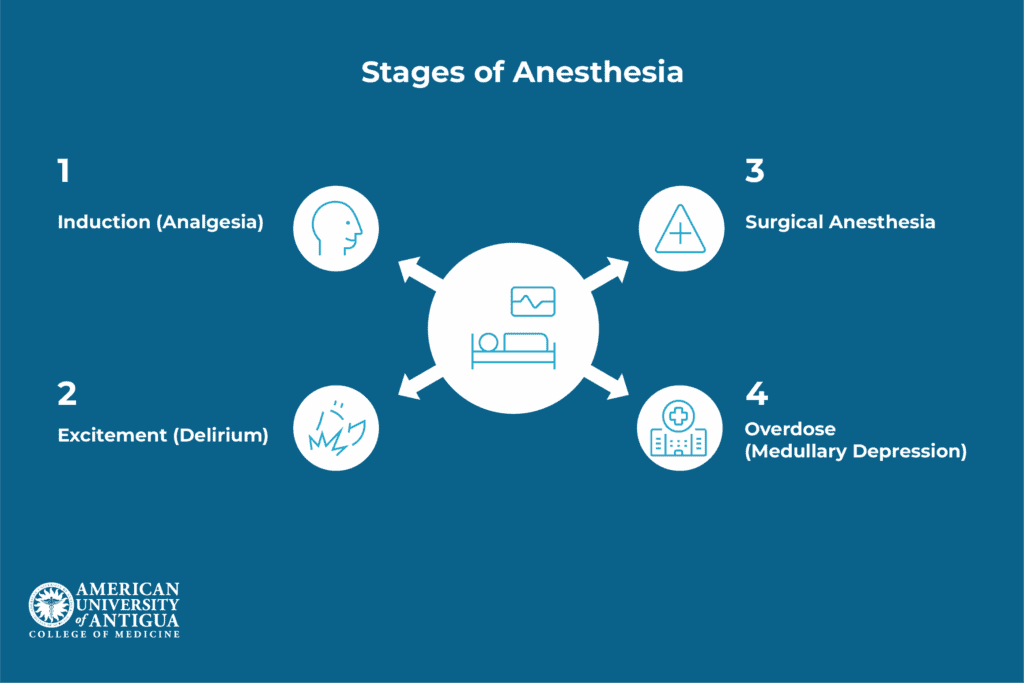
The concept of “stages” in anesthesia refers to distinct phases of consciousness and physiological response that occur as anesthetic agents take effect. These stages were originally described by Dr. Arthur Guedel in the early 20th century, specifically for anesthesia types using ether.
Guedel is often remembered for introducing the “Guedel chart” and even using an intubated dog named Airway to demonstrate safe anesthesia practices. His findings helped standardize anesthetic care at a time when it carried far greater risks.
While modern general anesthesia utilizes more sophisticated monitoring equipment and multiple drug combinations, Guedel’s classification system remains valuable for understanding patient responses during anesthetic administration. Each stage represents different levels of central nervous system depression and corresponding physiological changes.
Today’s anesthesiologists use these stages as a framework for recognizing patient status, even though contemporary practice involves more precise control through continuous monitoring and targeted drug delivery systems.
Stage 1 – Induction (Analgesia)
Stage 1 begins with anesthetic administration and continues until the patient loses consciousness. During this phase, patients experience drowsiness and significant pain relief while maintaining normal breathing patterns and protective reflexes.
Key characteristics of Stage 1 include:
- Conscious but drowsy state with maintained verbal response
- Effective analgesia allowing minor procedures without discomfort
- Normal breathing patterns and stable vital signs
- Intact protective reflexes including swallowing and coughing
Common induction agents used during this stage include propofol, etomidate, and sevoflurane, though specific choices depend on patient factors and surgical requirements. The duration of Stage 1 varies based on the anesthetic technique and individual patient response.
Anesthesiologists must carefully control this phase, since overly rapid induction can compromise the airway, while prolonged induction may increase patient discomfort or anxiety. From the patient’s perspective, this stage is often remembered as calm or even euphoric, which can be reassuring if explained beforehand.
This stage proves particularly useful for minor procedures, dental work, or as preparation for deeper anesthesia levels required for major surgery.
Stage 2 – Excitement (Delirium)
Stage 2 represents the transition period where patients lose consciousness but experience irregular physiological responses. This stage requires careful management due to increased risks of complications and unpredictable patient reactions.
During Stage 2, patients may exhibit:
- Loss of consciousness with unpredictable responses to stimuli
- Irregular breathing patterns that can compromise oxygenation
- Involuntary movements and muscle rigidity
- Heightened reflexes and potential for laryngospasm
Significant risks during this stage include vomiting, irregular heartbeat, and respiratory complications. Anesthesiologists work to minimize time spent in Stage 2 by using rapid-acting agents and smooth induction techniques.
Airway management becomes a key priority here, as laryngospasm and irregular breathing patterns pose real risks. Historically, this stage was much more prolonged with older anesthetics like ether, but modern drugs and muscle relaxants allow anesthesiologists to shorten or nearly bypass it altogether.
Pre-medication and careful drug selection help patients transition quickly through this potentially dangerous phase toward the stability of surgical anesthesia.
Stage 3 – Surgical anesthesia
Stage 3 provides optimal conditions for surgical procedures, with patients maintaining unconsciousness, stable breathing, and appropriate muscle relaxation. This stage is divided into four planes, ranging from light to deep surgical anesthesia.
Characteristics of Stage 3 include:
- Complete unconsciousness with no response to surgical stimulation
- Regular, adequate breathing maintained automatically
- Appropriate muscle relaxation allowing surgical access
- Stable vital signs with predictable physiological responses
The role of the anesthesiologist during Stage 3 involves continuous monitoring to make sure that patients remain at the appropriate depth for surgery while avoiding progression toward Stage 4. Modern anesthetic techniques allow precise control within this stage using multiple monitoring parameters.
Different surgical procedures require varying depths within Stage 3, with more invasive operations typically needing deeper anesthetic levels for optimal surgical conditions and patient comfort.
Stage 4 – Overdose (Medullary depression)
Stage 4 represents a dangerous level of anesthetic overdose that is never a goal of modern anesthesia practice. The name “medullary depression” comes from the suppression of the medulla oblongata in the brainstem, the region that controls essential functions such as breathing, heart rate, and blood pressure. When anesthetic depth reaches this stage, these vital centers slow down or stop functioning, leading to respiratory failure and cardiovascular collapse if not corrected immediately.
Based on that, some critical signs of Stage 4 include:
- Respiratory failure due to depression of breathing centers
- Cardiovascular collapse with severe blood pressure drops
- Absent reflexes and complete muscle flaccidity
- Potential cardiac arrest if not immediately corrected
Careful monitoring and precise drug administration prevent patients from reaching Stage 4. Modern anesthetic practice includes multiple safety systems, continuous vital sign monitoring, and immediate intervention protocols to maintain patient safety.
This stage is taught so anesthesiologists can recognize early warning signs and intervene immediately, even though it is not intended as part of modern practice. In the early history of anesthesia, Stage 4 occurred more often, but with today’s agents and monitoring, progression to this stage is extremely rare.
Recovery From Anesthesia
The recovery phase begins as soon as anesthetic agents are discontinued and patients gradually return to consciousness. This process essentially reverses the stages, with patients moving from Stage 3 back through Stage 2 and Stage 1 to full awakening.
Some common recovery symptoms from anesthesia include:
- Initial grogginess and disorientation as consciousness returns
- Potential nausea from anesthetic effects and surgical stress
- Sore throat from breathing tube placement during surgery
- Gradual return of normal reflexes and motor function
Safe awakening from anesthesia is a carefully managed process. As the surgery ends, anesthesiologists gradually reduce or discontinue anesthetic drugs so the patient begins to regain consciousness. During this period, they closely monitor vital signs such as heart rate, blood pressure, and oxygen levels to ensure stability. They also assess the patient’s level of consciousness, checking responsiveness to verbal or physical cues to confirm that awareness is returning appropriately.
Another critical step is confirming adequate breathing and airway function. Some patients may need assistance with ventilation until they can breathe effectively on their own, while others can resume normal breathing quickly. Only when these functions are stable do anesthesiologists allow patients to leave the operating room for the recovery area (PACU).
Recovery time varies considerably. Factors include the type of anesthetic drugs used (short-acting vs. longer-acting agents), the length and complexity of the surgery, and patient-specific considerations such as age, weight, or pre-existing health conditions. For example, a young, healthy patient may recover quickly from a short outpatient procedure, while an older patient with medical comorbidities might need longer monitoring.
Conclusion
Anyone aspiring to become an anesthesiologist must have a deep understanding of the stages of anesthesia and the responsibilities tied to each one. Even though this framework was developed many years ago, it remains highly relevant today. Modern anesthesia practice builds on these foundational concepts while adding advanced monitoring tools and precise drug delivery systems. Mastering these principles provides the essential groundwork for safe anesthetic care and the best outcomes for patients.
The role of an anesthesiologist is both demanding and rewarding, making it an excellent career path for those drawn to medicine. To pursue it, you need the right education and training. At the American University of Antigua College of Medicine (AUA), our MD program equips students with the knowledge and clinical experience they need to take on this responsibility with confidence. Find your specialty and then begin preparing for it with us at AUA.
Frequently Asked Questions
How long does anesthesia usually last?
The duration depends on the type of anesthesia and the surgery being performed; it can range from a few minutes for minor procedures to several hours for complex operations.
Is anesthesia safe for children and older adults?
Yes, anesthesia is considered safe for all ages when managed by trained professionals, though children and older adults require tailored drug choices and closer monitoring.
Can you wake up during surgery?
Awareness during surgery is extremely rare thanks to modern anesthetic techniques and monitoring, and anesthesiologists carefully adjust medications to prevent it.
✅ Request information on AUA's MD program TODAY!