Neurology Subspecialties: Areas, Focus, and Careers
Key Takeaways
- Neurology subspecialties offer focused expertise in specific areas of nervous system care.
- Each neurology subspecialty addresses distinct patient populations and conditions, allowing for targeted treatment approaches.
- Choosing a neurology subspecialty depends on your interest in patient demographics, work environment, and lifestyle preferences.
Neurology is a medical specialty that diagnoses and treats disorders of the brain, spinal cord, and nervous system. From stroke and epilepsy to Parkinson’s disease and multiple sclerosis, neurologists address conditions that affect how we move, think, and experience the world.
As our understanding of the nervous system grows, so does the need for specialized expertise. Neurology subspecialties meet this need by allowing doctors to focus deeply on specific patient groups and neurological conditions, developing advanced knowledge and skills in targeted areas of care.
✅ Request information on AUA's MD program TODAY!
Whether you’re drawn to acute care in the ICU, long-term management of chronic conditions, or working with children, understanding neurology subspecialties is the first step to discovering which path fits you best.
Major Neurology Subspecialties
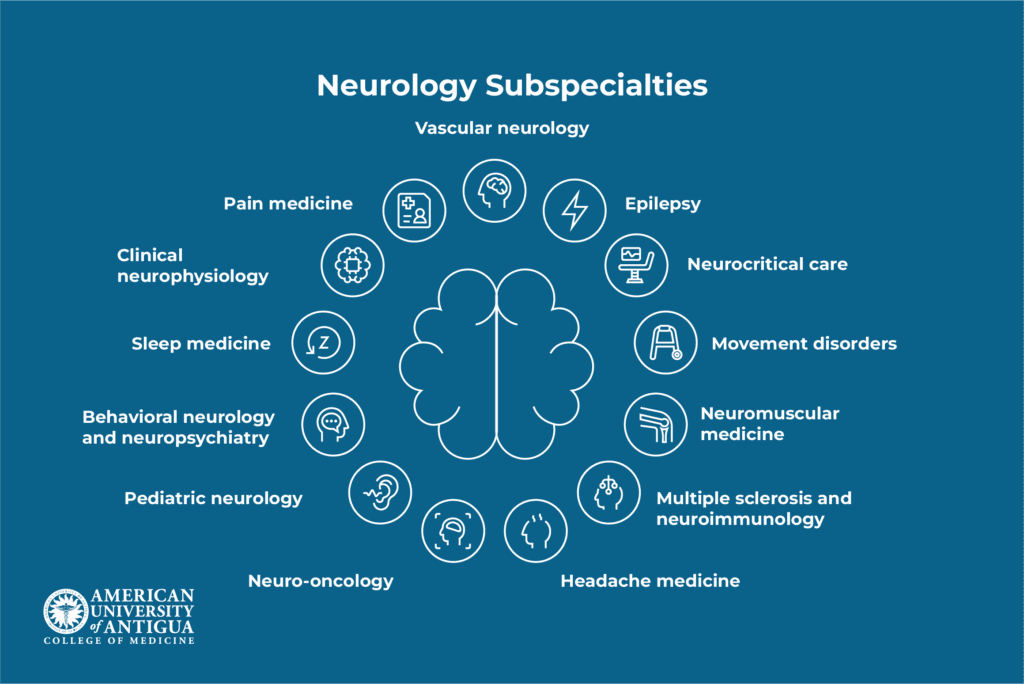
Subspecialization in neurology allows physicians to develop deeper expertise, contribute to cutting-edge research, and provide more targeted treatments for complex neurological conditions. After completing a neurology residency, doctors can pursue additional fellowship training (typically 1-2 years) in their chosen subspecialty.
Let’s explore the major neurology subspecialties, what they involve, and the career opportunities they offer.
Vascular neurology (stroke medicine)
Vascular neurologists specialize in cerebrovascular diseases, which are conditions affecting blood flow to the brain. This subspecialty focuses on preventing, diagnosing, and treating strokes and related disorders.
Key conditions treated:
- Ischemic stroke (caused by blood clots)
- Hemorrhagic stroke (caused by bleeding)
- Transient ischemic attacks (TIAs or “mini-strokes”)
- Carotid artery disease
- Cerebral aneurysms
Career paths: Vascular neurologists typically work in hospital settings, often in dedicated stroke centers where they respond to emergencies 24/7. Many also conduct research on stroke prevention and treatment innovations. According to recent data, stroke remains the second leading cause of death worldwide, making this subspecialty critically important.
The work is time-sensitive, as administering clot-busting medications within hours of symptom onset can mean the difference between recovery and permanent disability.
Epilepsy (neurophysiology)
Epilepsy specialists focus on seizure disorders and other conditions involving abnormal electrical activity in the brain. This subspecialty combines clinical care with sophisticated diagnostic testing.
Key conditions treated:
- Epilepsy (all types)
- Non-epileptic seizures
- Status epilepticus (prolonged seizures)
- Sleep-related seizure disorders
Career paths: Epileptologists work in both inpatient and outpatient settings. They interpret electroencephalograms (EEGs), conduct video-EEG monitoring, and manage complex medication regimens. Some specialize in epilepsy surgery evaluation, helping identify patients who might benefit from surgical treatment when medications fail.
Research opportunities abound in this field, from developing new anti-seizure medications to advancing surgical techniques. Approximately 1 in 26 people will develop epilepsy at some point in their lifetime, ensuring consistent demand for specialists.
Neurocritical care
Neurocritical care specialists manage life-threatening neurological emergencies in intensive care units (ICUs). This subspecialty blends neurology with critical care medicine.
Key conditions treated:
- Severe traumatic brain injury
- Brain hemorrhage
- Status epilepticus
- Brain infections (meningitis, encephalitis)
- Post-cardiac arrest brain injury
Career paths: Neurointensivists work exclusively in hospital ICUs, collaborating with neurosurgeons, emergency physicians, and critical care teams. The work involves managing ventilators, intracranial pressure monitors, and other life-support technologies.
This subspecialty suits those who thrive in high-acuity environments and enjoy procedural work alongside medical management. Many academic medical centers have dedicated neuro-ICUs staffed by specialists in this field.
Movement disorders
Movement disorder specialists focus on conditions affecting voluntary and involuntary movement. This includes some of the most recognizable neurological diseases.
Key conditions treated:
- Parkinson’s disease
- Essential tremor
- Dystonia (involuntary muscle contractions)
- Huntington’s disease
- Ataxia (coordination problems)
- Restless legs syndrome
Career paths: Movement disorder neurologists typically work in outpatient clinics, building long-term relationships with patients, while managing chronic conditions. Many participate in clinical trials testing new medications and therapies, including deep brain stimulation (DBS) programming.
The field offers opportunities to make meaningful differences in patients’ quality of life. With the aging population, the number of people with Parkinson’s disease is projected to rise significantly, reaching 1.2 million in the U.S. by 2030, with about 90,000 new cases each year.
Neuromuscular medicine
Neuromuscular specialists diagnose and treat diseases affecting muscles, peripheral nerves, and the connections between them.
Key conditions treated:
- Amyotrophic lateral sclerosis (ALS)
- Muscular dystrophy
- Myasthenia gravis
- Peripheral neuropathy
- Inflammatory myopathies
Career paths: These specialists perform specialized testing, including electromyography (EMG) and nerve conduction studies. They work in both clinic and electrodiagnostic laboratories, often serving as consultants for other physicians trying to diagnose muscle weakness or numbness.
The subspecialty requires patience and diagnostic skill, as neuromuscular conditions can be challenging to differentiate. Many specialists focus on either primarily nerve disorders or primarily muscle disorders within their practice.
Multiple sclerosis (MS) and neuroimmunology
This subspecialty focuses on autoimmune and inflammatory conditions affecting the nervous system. These are disorders where the immune system mistakenly attacks neural tissue.
Key conditions treated:
- Multiple sclerosis (MS)
- Neuromyelitis optica spectrum disorder (NMOSD)
- Autoimmune encephalitis
- Acute disseminated encephalomyelitis (ADEM)
- Guillain-Barré syndrome
Career paths: MS specialists typically work in outpatient MS centers, monitoring disease progression and adjusting disease-modifying therapies. The field has seen remarkable therapeutic advances in recent years, with numerous FDA-approved treatments now available.
Many specialists participate in clinical trials of emerging therapies. With approximately 2.9 million people living with MS worldwide, demand for specialized care continues to grow.
Headache medicine
Headache specialists focus on primary headache disorders and facial pain syndromes, helping patients who often struggle for years before finding effective treatment.
Key conditions treated:
- Migraine (episodic and chronic)
- Cluster headache
- Tension-type headache
- Trigeminal neuralgia
- Post-traumatic headache
Career paths: Most headache specialists work in outpatient settings, though some also provide inpatient consultations for patients with intractable headaches. Treatment involves medication management, nerve blocks, Botox injections, and newer therapies like CGRP monoclonal antibodies.
The field requires strong patient communication skills, as headache disorders significantly impact quality of life but don’t show up on standard imaging.
Neuro-oncology
Neuro-oncologists specialize in brain tumors and cancer-related neurological complications. This subspecialty bridges neurology, oncology, and neurosurgery.
Key conditions treated:
- Primary brain tumors (gliomas, meningiomas)
- Brain metastases from other cancers
- Paraneoplastic neurological syndromes
- Treatment-related neurotoxicity
- Seizures in cancer patients
Career paths: Neuro-oncologists work closely with neurosurgeons, radiation oncologists, and medical oncologists in multidisciplinary tumor boards. They manage both the tumors themselves and complications like seizures and cognitive changes.
Many work in academic medical centers conducting clinical trials of novel therapies. The field suits those comfortable with complex decision-making and providing compassionate care to patients facing serious diagnoses.
Pediatric neurology
Pediatric neurologists treat neurological conditions in infants, children, and adolescents (from newborns to young adults transitioning to adult care).
Key conditions treated:
- Epilepsy and seizure disorders
- Cerebral palsy
- Developmental delays
- Neurodevelopmental disorders (autism spectrum disorder, ADHD)
- Genetic neurological conditions
- Pediatric stroke
Career paths: Pediatric neurologists work in children’s hospitals and outpatient clinics, often subspecializing further in areas like pediatric epilepsy or neurodevelopmental disabilities. The work requires special skills in examining young children who can’t always describe their symptoms.
Many pediatric neurologists find the work particularly rewarding, as interventions during childhood can have profound long-term impacts. AUA graduates have matched into pediatric neurology residencies across multiple states, gaining experience in diverse clinical settings.
Behavioral neurology and neuropsychiatry
This subspecialty focuses on the intersection of neurology and psychiatry, treating conditions that affect cognition, behavior, and personality.
Key conditions treated:
- Alzheimer’s disease and other dementias
- Frontotemporal dementia
- Cognitive impairment following brain injury
- Behavioral changes from neurological disease
- Neuropsychiatric manifestations of movement disorders
Career paths: Behavioral neurologists often work in memory disorder clinics, performing detailed cognitive assessments and managing dementia care. The field requires strong communication skills for discussing sensitive diagnoses with patients and families.
With the aging population, dementia care represents a growing area of need. Many specialists conduct research on early detection and potential disease-modifying treatments for Alzheimer’s disease.
Sleep medicine
Sleep neurologists specialize in sleep disorders, which can have profound effects on health, safety, and quality of life.
Key conditions treated:
- Sleep apnea
- Narcolepsy
- Restless legs syndrome
- REM sleep behavior disorder
- Insomnia
- Circadian rhythm disorders
Career paths: Sleep specialists work in sleep centers, interpreting overnight sleep studies (polysomnography) and providing both medical and behavioral treatments. Many also see patients in clinics for follow-up care.
The field offers a relatively predictable lifestyle compared to some neurology subspecialties, with most work occurring during regular business hours. Sleep disorders are common, affecting up to 70 million Americans, yet often underdiagnosed.
Clinical neurophysiology
Clinical neurophysiologists focus on diagnosing neurological conditions using electrical and magnetic testing techniques.
Key conditions treated: This subspecialty is primarily diagnostic rather than treatment-focused, supporting diagnosis of:
- Epilepsy
- Nerve and muscle disorders
- Sleep disorders
- Brain death determination
- Intraoperative monitoring
Career paths: Neurophysiologists interpret EEGs, EMGs, nerve conduction studies, evoked potentials, and other neurophysiologic tests. Many work in electrodiagnostic laboratories and provide intraoperative monitoring during brain and spine surgeries.
The work is intellectually challenging and requires pattern recognition skills. It offers more predictable hours than many other subspecialties since testing is typically scheduled in advance.
Pain medicine
Pain neurologists specialize in chronic pain conditions, particularly those with neurological origins.
Key conditions treated:
- Neuropathic pain (nerve pain)
- Complex regional pain syndrome
- Chronic headache and facial pain
- Post-stroke pain
- Spinal pain syndromes
Career paths: Pain specialists use medication management, interventional procedures (nerve blocks, spinal injections), and multidisciplinary approaches, including physical therapy and psychological support.
The field requires patience and creativity, as chronic pain management often involves trial and error to find effective treatments. Many pain specialists work in dedicated pain clinics or multidisciplinary pain centers.
How to Choose a Neurology Subspecialty
Selecting a subspecialty is a personal decision that influences your daily work life and long-term career satisfaction. The main factors you need to consider when making your choice include the following:
- Patient population preferences: Do you prefer working with children, adults, or the elderly? Pediatric neurology and behavioral neurology serve very different age groups and needs.
- Work environment: Consider whether you’d perform best in hospital settings with acute care (neurocritical care, vascular neurology) or prefer outpatient clinics with longitudinal patient relationships (movement disorders, MS care).
- Procedures vs. cognitive work: Some subspecialties like clinical neurophysiology and pain medicine involve hands-on procedures, while others like behavioral neurology focus primarily on cognitive assessment and medication management.
- Lifestyle considerations: Emergency-focused subspecialties like stroke neurology often require night and weekend calls. Sleep medicine and headache medicine typically offer more regular hours.
- Research interests: If research appeals to you, consider fields with active clinical trial activity, like neuro-oncology, MS, and movement disorders.
The American University of Antigua College of Medicine provides a strong foundation for any neurology career path through its U.S.-modeled MD curriculum, which integrates theoretical knowledge with practical clinical experience.
Start a Career in Neurology
Neurology subspecialties offer diverse opportunities to make meaningful differences in patients’ lives; be it preventing strokes, managing epilepsy, or researching the next breakthrough in dementia care. Each subspecialty comes with unique challenges and rewards, from the fast-paced intensity of neurocritical care to the long-term relationships built in movement disorder clinics.
The path to becoming a neurologist requires dedication, but for those drawn to understanding the brain and nervous system, few fields offer such intellectual stimulation and clinical impact.
If you’re interested in a career in neurology, explore AUA’s MD program to learn how our curriculum, clinical partnerships, and global training opportunities can help you build a successful medical career.
Frequently Asked Questions (FAQs)
What is the hardest neurology subspecialty to get into?
Neurocritical care and vascular neurology fellowships are highly competitive due to limited positions and high demand, particularly at top academic medical centers.
What is the highest-paying neurology subspecialty?
Interventional neurology, pain medicine, and neurocritical care typically offer the highest compensation, though exact salaries vary by region, practice setting, and experience level.
How long does it take to become a neurologist?
It takes 11-12 years after high school: four years undergraduate, four years medical school, and at least three years neurology residency, plus 1-2 additional years for subspecialty fellowship training.
✅ Request information on AUA's MD program TODAY!