Nephrologist vs. Urologist – Differences and Similarities
Understanding medical specialties is crucial for patients seeking appropriate and effective healthcare. In the realm of kidney and urinary tract health, distinguishing between a nephrologist and a urologist is particularly important. Nephrologists specialize in diagnosing and providing treatment for kidney diseases, focusing on chronic kidney disease, hypertension, and electrolyte imbalances. Urologists, on the other hand, address surgical and non-surgical issues related to the urinary tract and male reproductive system, including kidney stones, bladder problems, and prostate issues. Recognizing the differences and similarities between these two specialties ensures that patients receive targeted care from the right healthcare provider, ultimately improving treatment outcomes and overall well-being.
What Is a Urologist?
A urologist is a medical expert who manages conditions affecting both the urinary tract and the male reproductive system. Urology primarily focuses on managing conditions affecting the kidneys, bladder, urethra, and ureters, as well as addressing issues related to the male reproductive organs, including the prostate, testes, and penis. Urologists manage a wide range of conditions, such as urinary tract infections, kidney stones, bladder control problems, and prostate issues. Common procedures performed by urologists include:
✅ Request information on AUA's MD program TODAY!
YOUR PATH TO SUCCESS BEGINS HERE
- Cystoscopy (examining the bladder and urethra);
- Lithotripsy (breaking up kidney stones);
- Prostate biopsies;
- Surgeries to remove tumors or repair urinary tract obstructions.
Urologists are essential in maintaining urinary and reproductive health, managing both the medical and surgical aspects of these conditions.
What Is a Nephrologist?
A nephrologist is a physician who focuses on diagnosing and treating kidney-related diseases and conditions. Nephrology primarily focuses on managing kidney-related disorders, including chronic kidney disease, acute kidney injury, glomerulonephritis, and electrolyte imbalances. Nephrologists are also experts in hypertension, as high blood pressure is closely linked to kidney health. Common procedures and tests conducted by nephrologists include:
- Kidney biopsies;
- Dialysis (both hemodialysis and peritoneal dialysis);
- Various blood and urine tests to assess kidney function and electrolyte levels.
Additionally, nephrologists often work with patients who have undergone kidney transplantation, providing long-term care and management to ensure the success of the transplant. Through these specialized practices, nephrologists play a crucial role in preserving kidney health and overall well-being.
Education Requirements for Nephrologists vs. Urologists
To understand the distinction between a nephrologist and a urologist, it is essential to recognize the unique educational pathways required for each specialty. Both professions require extensive training and education. This rigorous training ensures that each specialist is well-equipped to provide expert care in their respective fields, addressing the distinct needs of patients with kidney and urinary tract issues.
Nephrologist training
Becoming a nephrologist starts with obtaining a bachelor’s degree in a medical-related field. Afterward, aspiring nephrologists need to go through four years of medical school to earn a medical degree. After graduation, future nephrologists must complete a three-year internal medicine residency to gain foundational knowledge and clinical experience. This is followed by a two to three-year nephrology fellowship specializing in kidney diseases, electrolyte disorders, hypertension, and renal replacement therapies such as dialysis and kidney transplantation.
Board certification in nephrology is typically obtained after completing the fellowship training and passing the certification examination administered by the American Board of Internal Medicine (ABIM). Certification demonstrates a nephrologist’s competence and commitment to maintaining high standards of medical practice in nephrology, ensuring they are well-prepared to provide comprehensive care to patients with kidney-related conditions.
Urologist training
Becoming a urologist involves a rigorous educational pathway, starting with obtaining a bachelor’s degree in a medical-related field. Afterwards, aspiring urologists also go through four years of medical school to earn a medical degree. Different from nephrologists, future urologists need to enter a five to six-year urology residency program after medical school to gain comprehensive training in surgical and non-surgical management of urinary tract and male reproductive system conditions. This includes diagnosing and treating kidney stones, UTIs, prostate diseases, and urological cancers, emphasizing hands-on surgical experience under experienced urologists. Regarding fellowship training, individuals may or may not choose to pursue it for further specialization since it is not required to practice general urology.
Board certification in urology is obtained after completing the residency training and passing the certification examination administered by the American Board of Urology (ABU). Certification demonstrates that a urologist has met rigorous standards of knowledge, skill, and experience in urological care, affirming their ability to provide high-quality care to patients with urological conditions. This certification is essential for urologists seeking to practice independently and demonstrate their commitment to excellence in the field of urology.
Roles and Responsibilities for Nephrologists and Urologists
Understanding the distinct roles and responsibilities of nephrologists and urologists is crucial for patients seeking specialized care for kidney and urinary tract conditions. In the following paragraphs, we will delve into their specific duties, expertise, and contributions to patient care, highlighting how each specialist plays a vital role in addressing complex medical needs related to renal health and urological disorders.
Nephrologist roles
Nephrologists specialize in diagnosing and managing kidney-related diseases and conditions, focusing on preserving kidney function and overall health. They are experts in managing chronic kidney diseases (CKD) through medical interventions to slow disease progression and prevent complications. Nephrologists also oversee the treatment of acute kidney injuries (AKI), glomerulonephritis, and electrolyte imbalances that affect kidney function. Their expertise includes managing hypertension, a major risk factor for kidney disease, and providing renal replacement therapies, including dialysis and kidney transplantation, for those with end-stage kidney failure. Nephrologists aim to enhance patient outcomes and quality of life by providing comprehensive care for kidney-related challenges.
Urologist roles
Urologists are focused on diagnosing and providing treatment for disorders affecting the urinary tract and male reproductive system. They specialize in treating conditions such as urinary tract infections, bladder problems, such as urinary incontinence, and prostate disorders, which encompass benign prostatic hyperplasia (BPH) and prostate cancer. Urologists also perform a wide range of surgical procedures, ranging from minimally invasive techniques like prostate surgery (such as TURP) to complex surgeries such as kidney stone removal (via procedures like lithotripsy or ureteroscopy) and bladder cancer treatment, ensuring comprehensive care tailored to each patient’s needs.
Common Conditions Treated by Nephrologists vs. Urologists
Nephrologists and urologists specialize in managing distinct medical conditions related to kidney health and urinary tract disorders. In the following paragraphs, we will delve into the common conditions each specialty addresses, highlighting their expertise in diagnosing, treating, and managing them to ensure optimal patient care and health outcomes.
Conditions treated by nephrologists
Nephrologists specialize in diagnosing and managing various kidney-related conditions that affect overall health and well-being. They are experts in chronic kidney disease (CKD), which involves a progressive loss of kidney function over time, and acute kidney injury (AKI), which can occur suddenly due to various factors such as infections or medication reactions. Nephrologists also treat glomerulonephritis, an inflammation of the kidney’s filtering units, and electrolyte imbalances that can arise from kidney dysfunction. Additionally, they manage conditions like hypertension that can both contribute to and result from kidney disease. While nephrologists do not perform surgical interventions for kidney stones, they play a crucial role in the medical management and prevention of these and other kidney-related issues.
Conditions treated by urologists
Urologists specialize in diagnosing and managing various conditions affecting the urinary tract and male reproductive system. They manage urinary tract infections (UTIs), which can affect the kidneys, bladder, ureters, and urethra. Urologists also address bladder issues such as overactive bladder and urinary incontinence, providing both medical and surgical interventions. Prostate conditions fall within their expertise, including benign prostatic hyperplasia (BPH) and prostate cancer, with treatments ranging from medication to minimally invasive surgical procedures. Urologists also play a role in addressing male infertility through diagnostic evaluations and treatments such as surgical sperm retrieval. Additionally, they specialize in managing kidney stones, using procedures like lithotripsy to break down stones or performing surgical removal when necessary, ensuring comprehensive care for patients with urological conditions.
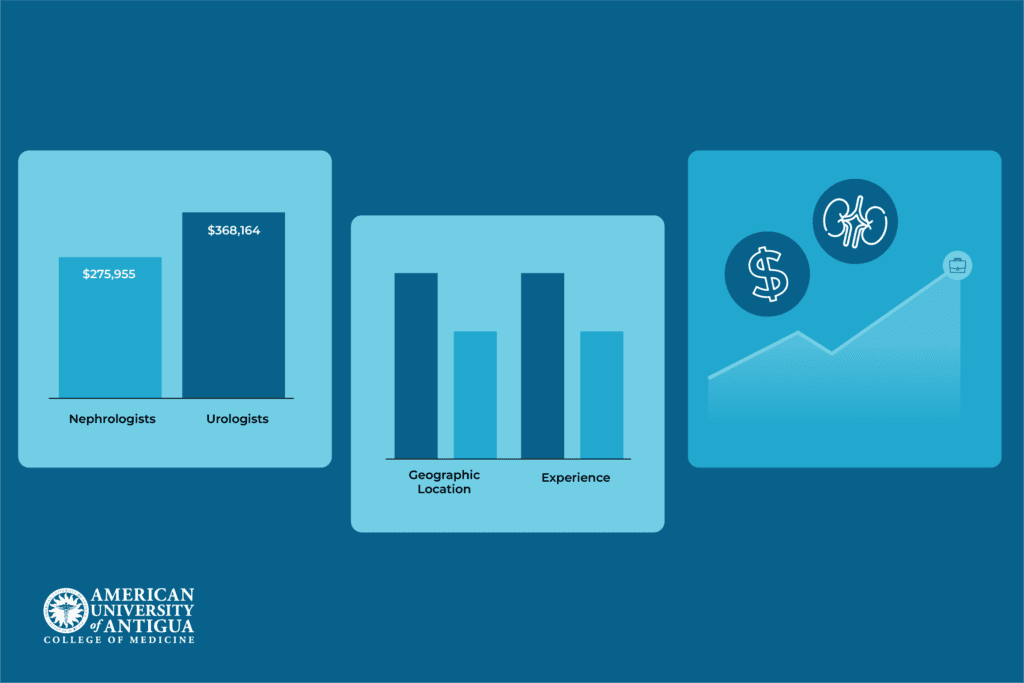
Salary Comparisons and Job Outlook: Nephrologists vs. Urologists
Salary comparisons between nephrologists and urologists in the United States highlight significant differences reflecting their specialties. As of July 11, 2024, nephrologists earn an average annual salary of approximately $275,955, while urologists command a higher yearly average wage of around $368,164. Geographic location influences salaries, with urban areas typically providing higher compensation due to higher living costs and greater demand for specialized medical care. Experience and subspecialty expertise further influence earning potential in both fields. Both nephrologists and urologists are expected to experience demand for their services, with overall employment for physicians and surgeons projected to increase by 3% from 2022 to 2032. This growth is largely fueled by an aging population and increasing healthcare needs related to kidney and urological disorders.
Choosing Between Nephrology and Urology: Key Considerations
When choosing between a career in nephrology or urology, consider how each aligns with your interests and goals. Nephrology focuses on renal physiology and kidney function, addressing conditions like chronic kidney disease and hypertension, and requires meticulous attention to chronic conditions. Urology is suited for those interested in surgical interventions and treating a variety of urinary tract and male reproductive system disorders, including kidney stones and prostate issues.
Lifestyle differences are also significant in the decision-making process. Nephrologists generally have a predictable schedule with fewer urgent surgeries, while urologists face varied surgical demands and on-call duties. Nephrologists typically work in outpatient clinics, hospitals, or dialysis centers, whereas urologists work in surgical settings, clinics, or academic institutions. Nephrologists often build long-term relationships with patients managing chronic conditions, while urologists handle acute and chronic patient care needs.
Ultimately, the decision between nephrology and urology should align with personal interests, strengths, and career aspirations, ensuring a fulfilling and rewarding professional journey in either specialized medical field.
Conclusion
Understanding the differences between nephrologists and urologists is crucial for patients seeking specialized care. Whether managing kidney diseases or urinary tract disorders, each specialty offers unique expertise.
Explore the American University of Antigua (AUA) College of Medicine for comprehensive urology and nephrology programs and embark on a fulfilling career in these vital medical fields.
Frequently Asked Questions
How do nephrologists and urologists work together?
Nephrologists and urologists collaborate to provide comprehensive care for patients with kidney and urinary tract disorders, ensuring both medical management and surgical interventions are optimized.
How long does it take to become a nephrologist or urologist?
It typically takes 13-14 years of education and training after high school to become a nephrologist, including the bachelor’s degree program, medical school, residency, and fellowship. Meanwhile, becoming a urologist requires 13-14 years only for the bachelor’s degree program, medical school, and residency. If one wants to pursue a fellowship for further specialization, an additional 1-2 years are required.
Can nephrologists and urologists prescribe medications?
Yes, both nephrologists and urologists are licensed physicians who can prescribe medications as part of their patient treatment plans.
✅ Request information on AUA's MD program TODAY!