Medical Ethics: Key Principles & Ethical Dilemmas
Key Takeaways
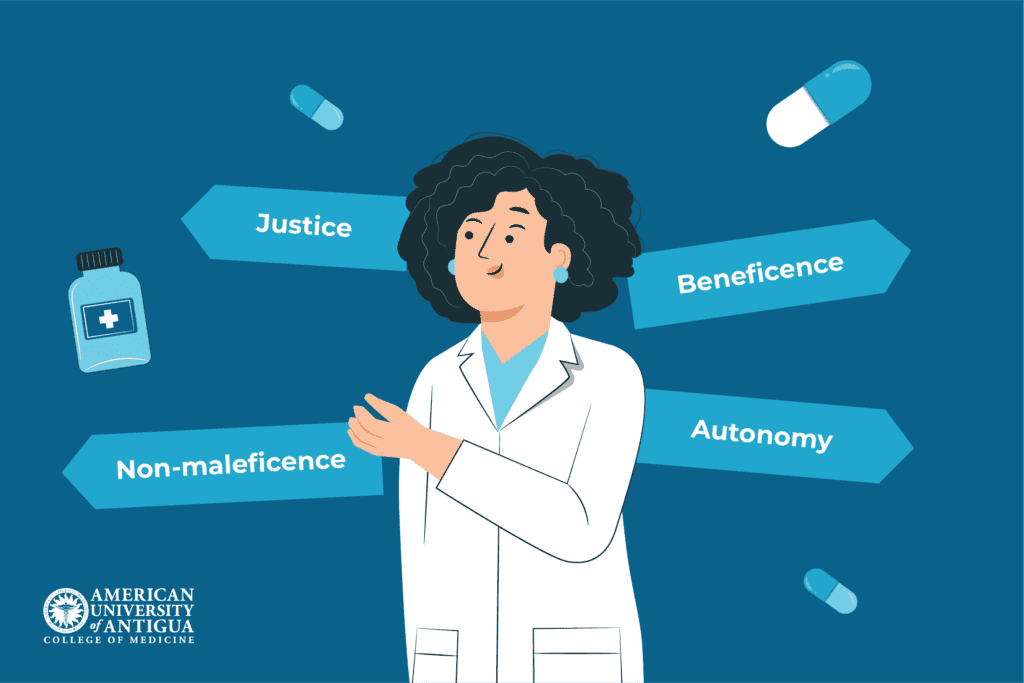
- Medical ethics is built on four key principles: autonomy, beneficence, non-maleficence, and justice.
- Ethical dilemmas arise in areas like end-of-life care, patient confidentiality, informed consent, and resource allocation, requiring a balance between patient rights and medical responsibility.
- Bioethics addresses modern challenges, including AI in medicine, gene editing, and the ethical implications of cloning and stem cell research.
- A strong understanding of medical ethics is essential for practicing medicine with integrity, compassion, and fairness.
Medical ethics has shaped healthcare for centuries, guiding doctors through difficult decisions. It dates back to Hippocrates, whose famous oath laid the foundation for ethical medical practice. While “do no harm” remains a core principle, modern medicine presents challenges Hippocrates could never have imagined, including AI-driven diagnoses, gene editing, and end-of-life care.
Today, ethical principles like autonomy, beneficence, non-maleficence, and justice help doctors navigate these complexities. Ethical dilemmas arise daily, from patient confidentiality to resource allocation, requiring careful judgment. This article explores the key principles of medical ethics, real-world dilemmas, and the evolving role of bioethics in shaping the future of medicine.
✅ Request information on AUA's MD program TODAY!
What Is Medical Ethics?
Medical ethics build the foundation of responsible healthcare, ensuring that medical decisions prioritize patient well-being, fairness, and moral integrity. It guides doctors, nurses, researchers, and policymakers in navigating complex situations, balancing scientific advancements with human values.
In clinical care, medical ethics shapes how providers respect patient autonomy, maintain confidentiality, and ensure fair treatment. In research, it ensures studies are conducted safely, ethically, and with informed consent. Ethical principles also guide medical policies, establishing guidelines that benefit society while protecting individual rights. Meanwhile, public health ethics address broader issues like vaccine distribution and disease prevention.
Institutions such as medical associations, bioethics committees, and hospital ethics boards play a crucial role in upholding these standards. The World Medical Association (WMA) and the American Medical Association (AMA) establish global and national ethical guidelines, while hospital ethics boards provide case-specific guidance. These frameworks help maintain accountability, ensuring ethical integrity in all aspects of medicine.
The Four Pillars of Medical Ethics
Modern medical ethics is grounded on four key principles: autonomy, beneficence, non-maleficence, and justice. These principles serve as guiding pillars for ethical decision-making, helping healthcare professionals navigate complex situations while ensuring patient rights, safety, and fairness remain at the core of medical practice and policy.
Autonomy
Autonomy refers to the patient’s right to make their own healthcare decisions. This principle honors individual freedom, ensuring that medical choices reflect a patient’s values, beliefs, and preferences. Informed consent is a key aspect of autonomy. Healthcare providers must offer patients detailed information about treatment options, risks, and benefits to help them make educated decisions.
In practice, autonomy is pivotal in cases like end-of-life decisions, refusal of treatment, or selecting elective procedures. For example, a cancer patient may decline chemotherapy despite its potential benefits. Respecting autonomy means honoring this decision, even if the doctor personally disagrees.
Beneficence
Beneficence requires that healthcare providers act in the patient’s best interest, promoting well-being and positive outcomes. It goes beyond avoiding harm, requiring active efforts to do good – from recommending the most effective treatments to providing compassionate care.
For instance, a doctor treating a stroke patient might advocate for aggressive rehabilitation, understanding its long-term recovery benefits. In research, beneficence ensures that clinical trials serve the interests of participants and contribute to future medical progress. Without this principle, medical practice risks becoming overly impersonal, treating patients as mere subjects of clinical trials rather than individuals with unique needs.
Non-maleficence
Non-maleficence means “do no harm.” Healthcare providers must avoid causing unnecessary suffering, even when trying to help the patient. They should carefully weigh the potential risks and benefits of treatments and interventions to ensure ethical decision-making.
A common example is opioid prescriptions. While pain management is essential, excessive use of opioids can lead to addiction. A doctor practicing non-maleficence would seek safer pain management options before resorting to high-risk medications. Similarly, in surgery, minimally invasive techniques are preferred over more aggressive procedures to minimize complications and risks.
Justice
Justice in medical ethics ensures fairness in the distribution of healthcare resources, access to treatment, and decision-making. This principle requires that care is provided without discrimination, balancing individual needs with the broader societal context.
For example, in the case of organ transplants, justice ensures recipients are chosen based on medical urgency rather than wealth or social status. In public health initiatives, such as vaccine distribution, justice ensures that priority is given to populations at higher risk.
Justice also plays a significant role in combating healthcare inequalities, advocating for equal treatment regardless of race, gender, or socioeconomic background. Without justice, healthcare systems risk favoring the privileged over the vulnerable.
Common Ethical Dilemmas in Healthcare
Ethical dilemmas arise when healthcare professionals face conflicting moral principles, making it challenging to choose the best course of action. Common dilemmas include end-of-life decisions, patient confidentiality vs. public safety, resource allocation, and informed consent challenges. These situations require careful ethical reasoning to balance patient rights and medical responsibility.

End-of-life decisions
End-of-life care presents complex ethical challenges, especially in cases of euthanasia, physician-assisted suicide, and Do Not Resuscitate (DNR) orders. While patient autonomy must be respected, healthcare providers also need to consider beneficence (acting in the patient’s best interest) and non-maleficence (avoiding harm).
A notable example is the Charlie Gard case, where doctors and parents clashed over whether to continue life support for a terminally ill infant. The hospital argued that further treatment would only cause unnecessary suffering, while the parents wanted to try experimental therapy. The case highlighted the difficult balance between medical judgment, ethical principles, and respecting family wishes in critical care decisions.
Patient confidentiality
Protecting patient confidentiality is a fundamental ethical obligation in healthcare, fostering trust between patients and providers. In the U.S., laws like the Health Insurance Portability and Accountability Act (HIPAA) protect personal health information. However, confidentiality isn’t absolute — exceptions are made when public safety is at risk.
Healthcare providers may be required to breach confidentiality in cases of infectious disease reporting, threats of harm to others, or child abuse. An example is the Tarasoff case, where a psychologist failed to warn a woman about a patient’s violent threats, which led to her murder. This case shaped laws requiring mental health professionals to warn potential victims, balancing privacy with the need for public protection.
Informed consent
Informed consent is the practice of providing patients with detailed, comprehensive information about a medical procedure – including its risks, benefits, and alternatives – before they agree to it. This process upholds patient autonomy, allowing individuals to make educated decisions about their healthcare. Without informed consent, medical treatment can become unethical, or even illegal.
Challenges arise when patients cannot provide informed consent, such as minors, unconscious individuals, or those with severe mental impairments. In these cases, legal guardians or healthcare proxies make decisions guided by hospital policies and ethical principles.
A well-known case is that of Henrietta Lacks, whose cells were used for groundbreaking medical research without her consent. This ethical violation sparked major discussions on patient rights and helped shape modern consent laws, ensuring patients have control over their own medical decisions.
Allocation of resources
When medical resources such as ICU beds, ventilators, or organ transplants are limited, ethical dilemmas arise. Who gets priority? Decisions must balance medical urgency, likelihood of survival, and fairness, ensuring no one is discriminated against due to socioeconomic status or personal background.
Public health emergencies, like the COVID-19 pandemic, caused critical resource shortages, requiring doctors to decide who would receive life-saving care. Ethical frameworks guided these decisions, prioritizing those with the best chances of survival.
A striking example occurred during the COVID-19 crisis in Italy, where overwhelmed hospitals had to ration ventilators. Doctors followed triage protocols, prioritizing younger and healthier patients, sparking global debates on fairness in crisis decision-making. These situations highlight the need for ethical policies that ensure life-saving resources are distributed justly, even in dire circumstances.
The Role of Bioethics in Modern Medicine
Bioethics is a field that examines the ethical, legal, and social implications of advancements in medicine and biotechnology. While traditional medical ethics focuses on patient care and professional conduct, bioethics tackles broader issues related to technology, research, and societal impact.
One major concern in bioethics is the integration of AI in medicine. AI-powered systems assist in diagnosis and treatment, but ethical challenges arise regarding decision-making responsibility, patient data privacy, and algorithmic bias. For example, if an AI system misdiagnoses a patient, who bears responsibility – the developer or the physician?
Another controversial area is gene editing, particularly CRISPR technology. While it offers potential cures for genetic diseases, it also raises concerns about human DNA modifications, the possibility of “designer babies,” and unintended social inequalities.
Bioethics also navigates the moral and legal dilemmas surrounding cloning and embryonic stem cell research. While these advancements offer groundbreaking medical opportunities, they spark debates over the sanctity of life and the ethical limits of scientific intervention.
As medicine advances, bioethics ensures that innovation aligns with ethical principles, balancing progress with moral responsibility. Without ethical oversight, scientific breakthroughs risk outpacing ethical considerations, leading to unintended harm.
Conclusion
Medical ethics guides healthcare professionals in making fair, compassionate, and responsible decisions. Grounded in the principles of autonomy, beneficence, non-maleficence, and justice, it helps navigate complex dilemmas like end-of-life care, patient confidentiality, informed consent, and resource allocation. As medicine advances, bioethics ensures that advancements like AI, gene editing, and cloning align with ethical values.
A strong understanding of medical ethics is crucial for any future physician. At AUAMED, students gain the knowledge and skills to tackle real-world ethical challenges with confidence. If you’re passionate about medicine and integrity, applying to AUAMED’s medical school is the first step in your journey. Become the doctor patients can trust!
Frequently Asked Questions
Can a doctor refuse to treat a patient for ethical reasons?
Yes, but only in specific situations. Doctors cannot refuse treatment based on discrimination. They can only do so if it goes against their ethical beliefs (e.g., assisted suicide), poses a risk to their safety, or if another provider is better suited to the patient’s needs. In such cases, they must ensure the patient has access to alternative treatment.
What happens when a doctor violates medical ethics?
Consequences are determined by the severity of the violation. Minor breaches may lead to warnings or additional training, while serious offenses, like malpractice or patient harm, can result in license suspension, lawsuits, or even criminal charges. Ethical violations can also permanently damage a doctor’s reputation and career.
✅ Request information on AUA's MD program TODAY!