Immunologist vs. Rheumatologist – Learn the Key Differences
It is essential to understand the distinct roles of immunologists and rheumatologists to make informed decisions about your health or the career path you want to pursue. Both immunologists and rheumatologists play vital roles in diagnosing and treating various conditions. However, their areas of expertise differ significantly. Immunologists specialize in the immune system, addressing allergies, autoimmune diseases, and immunodeficiencies. Meanwhile, rheumatologists focus on musculoskeletal disorders and autoimmune diseases affecting the joints, muscles, and bones.
This blog aims to illuminate the key differences between these two specialties, helping you navigate your healthcare and career choices with confidence and clarity.
✅ Request information on AUA's MD program TODAY!
YOUR PATH TO SUCCESS BEGINS HERE
What Is an Immunologist?
An immunologist is a medical specialist dedicated to understanding and treating disorders related to the immune system. Their expertise encompasses various conditions, including immune system disorders, allergies, and autoimmune diseases. Immunologists focus on diagnosing and managing diseases where the immune system is overactive, such as in allergies and autoimmune diseases like lupus and rheumatoid arthritis, or underactive, as in immunodeficiencies. These specialists often work in diverse settings, including laboratories, hospitals, and research institutions, where they conduct tests, develop treatments, and advance our understanding of the immune system by conducting groundbreaking research.
What Is a Rheumatologist?
A rheumatologist is a medical expert focused on diagnosing and managing conditions that affect the joints, muscles, and bones. Their expertise extends to various conditions, including arthritis, osteoporosis, lupus, and other autoimmune disorders that affect the musculoskeletal system. Rheumatologists are adept at managing chronic pain, inflammation, and the complexities of autoimmune diseases that can severely impact a patient’s quality of life. Typically, these specialists work in clinics, hospitals, and private practices, providing comprehensive care through patient consultations, diagnostic testing, and long-term management plans tailored to each individual’s needs.
Differences Between Immunologists and Rheumatologists
While both immunologists and rheumatologists play critical roles in healthcare, their expertise and focus areas differ significantly. To fully understand these distinctions, exploring various aspects of their professions, including education, training, conditions treated, treatment methods, skills, and salary, is essential.
In the following paragraphs, we will delve into these key differences, providing a comprehensive comparison to help you better appreciate the unique contributions of each specialty to patient care.
Education and training
Both immunologists and rheumatologists undergo rigorous education and training to specialize in their respective fields. The path to becoming an immunologist generally begins with earning a bachelor’s degree, followed by four years in medical school to obtain a Doctor of Medicine (M.D.) or Doctor of Osteopathic Medicine (D.O.) degree. After completing medical school, aspiring immunologists undergo a residency program in internal medicine or pediatrics, lasting three years, to acquire foundational clinical skills. Following residency, they may pursue a fellowship in immunology, ranging from two to three years, focusing on specialized training in immune system disorders, allergies, and autoimmune diseases.
Rheumatologists also begin with obtaining a bachelor’s degree and completing four years of medical school to earn an M.D. or D.O. degree. After medical school, they undertake a residency program in internal medicine or pediatrics, similar to immunologists, lasting three years. However, rheumatologists then pursue a fellowship specifically in rheumatology, typically lasting two to three years. During this fellowship, they gain expertise in diagnosing and treating joints, muscles, and bone disorders, including autoimmune conditions like arthritis and lupus. This focused training prepares rheumatologists to deliver thorough care to individuals dealing with intricate musculoskeletal and autoimmune conditions.
Conditions treated
Immunologists specialize in diagnosing and treating a wide range of immune system-related conditions. Common disorders addressed by immunologists include allergies (such as asthma, hay fever, and food allergies), autoimmune diseases (like rheumatoid arthritis, lupus, and multiple sclerosis), and immunodeficiencies (such as HIV/AIDS and primary immunodeficiency disorders). They also manage conditions involving abnormal immune responses, such as inflammatory bowel disease (IBD) and transplant rejection.
Conversely, rheumatologists focus primarily on disorders affecting the joints, muscles, and bones. Rheumatologists treat conditions such as various types of arthritis (e.g., rheumatoid arthritis, osteoarthritis, and gout), autoimmune diseases affecting joints (like systemic lupus erythematosus), osteoporosis, and musculoskeletal pain syndromes.
There are several overlapping conditions for which both specialties may collaborate in treatment. For instance, autoimmune diseases like lupus or rheumatoid arthritis involve immune system dysfunction and musculoskeletal symptoms, requiring coordinated care between immunologists and rheumatologists. Collaborative approaches may involve combining immunosuppressive therapies with treatments to manage joint inflammation and pain. This multidisciplinary approach ensures comprehensive care tailored to the complex needs of patients with overlapping conditions.
Treatment methods
Immunologists employ a variety of treatment approaches depending on the specific immune-related disorder. For allergies, treatments may include allergen immunotherapy (commonly known as allergy shots) to desensitize the immune system to specific allergens. Immunologists also prescribe antihistamines, corticosteroids, and biological therapies to manage allergic reactions and autoimmune diseases. In cases of immunodeficiency disorders, treatments often involve immunoglobulin replacement therapy or medications to boost immune function. A highly individualized approach focuses on addressing the underlying immune system dysfunction while minimizing adverse effects.
Rheumatologists utilize diverse strategies to manage conditions affecting the joints, muscles, and bones. Common treatments include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): to reduce inflammation and pain;
- Disease-modifying antirheumatic drugs (DMARDs): to slow the progression of autoimmune diseases like rheumatoid arthritis;
- Biologic therapies: to target specific components of the immune system.
Additionally, rheumatologists may recommend physical therapy to improve joint function and mobility and perform joint injections with corticosteroids or hyaluronic acid to alleviate pain and inflammation directly at the affected site. Treatment plans are tailored meticulously to each patient’s symptoms, disease severity, and overall health status, aiming to achieve optimal outcomes and enhance quality of life.
Both specialties emphasize personalized care, considering factors such as patient preferences, coexisting medical conditions, and potential side effects of treatments. Collaboration between immunologists and rheumatologists may be necessary for patients with complex conditions involving immune system dysfunction and musculoskeletal manifestations, ensuring a comprehensive and coordinated approach to treatment.
Skills
Immunologists rely on analytical skills, attention to detail, and problem-solving abilities to manage the complexities of immune-related disorders effectively. They must possess strong research skills to investigate and understand intricate immune system mechanisms, often employing advanced laboratory techniques and interpreting complex data. Attention to detail is crucial in diagnosing and monitoring conditions like allergies and autoimmune diseases, where subtle changes in immune responses can significantly impact patient outcomes. Effective problem-solving skills allow immunologists to develop innovative treatment approaches tailored to individual patient needs, addressing both acute symptoms and long-term management of chronic immune disorders.
Rheumatologists require diverse skills to diagnose and manage disorders affecting the musculoskeletal system. Patient communication skills are paramount, as rheumatologists must effectively communicate complex medical information and treatment options to patients and their families. Manual dexterity is essential for performing precise joint examinations and procedures, such as injections or aspirations, ensuring accurate diagnosis and treatment delivery. Diagnostic skills are also critical, enabling rheumatologists to differentiate between various types of arthritis and autoimmune diseases based on clinical evaluations, laboratory tests, and imaging studies. Additionally, rheumatologists must possess strong interdisciplinary collaboration skills to work closely with other healthcare professionals, such as physical and occupational therapists, to optimize patient care and outcomes.
Salary
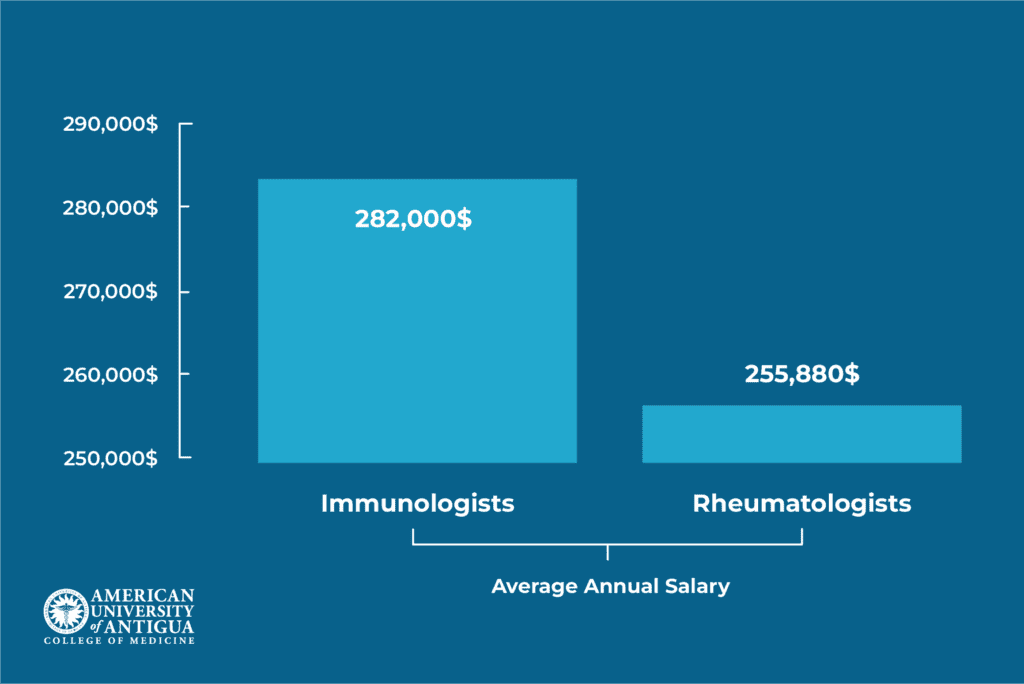
As of June 27, 2024, the average salary for immunologists in the United States is $282,000 annually. In comparison, rheumatologists earn an average salary of $255,880 per year. Salary figures can vary significantly based on several factors, including geographic location, experience level, type of practice (academic, private, or research), and additional certifications or specialties. Immunologists and rheumatologists working in metropolitan areas or regions with higher living costs generally command higher salaries. Professionals with extensive experience, advanced academic credentials, or leadership positions in their field may earn salaries at the higher end of these ranges. Understanding these factors can help professionals in these fields make informed decisions about their career paths and practice locations.
Immunologist vs. Rheumatologist: Which One Should You Choose?
Choosing between becoming an immunologist or a rheumatologist depends on several key factors that prospective medical professionals should carefully consider. Personal interests play a crucial role; those interested in exploring the complex mechanisms of the immune system and managing conditions such as allergies, autoimmune diseases, and immunodeficiencies may find a career in immunology particularly rewarding. Conversely, individuals passionate about diagnosing and treating musculoskeletal conditions such as arthritis, lupus, and osteoporosis may lean towards rheumatology. Career goals also matter, as immunologists often engage in research and laboratory work, while rheumatologists typically focus on clinical practice and diagnosing and treating patients directly.
The pros and cons of each specialty also weigh in the decision-making process. Immunologists have the chance to lead pioneering research efforts, pushing forward our understanding and treatment of disorders related to the immune system. However, this often involves extended periods in laboratories and research settings. On the other hand, rheumatologists directly interact with patients, providing hands-on care and witnessing tangible improvements in quality of life. They may find fulfillment in long-term patient relationships but must navigate the challenges of managing chronic conditions.
For students and aspiring medical professionals, it’s essential to consider the job outlook and demand for each specialty. Immunologists and rheumatologists are both integral to healthcare, with growing demands driven by aging populations and the increasing prevalence of immune-related and musculoskeletal disorders. Researching educational requirements and training pathways and exploring opportunities for specialization or dual certification can provide clarity when choosing between these rewarding medical specialties.
Conclusion
In conclusion, understanding the differences between immunologists and rheumatologists highlights their distinct roles in healthcare. Immunologists specialize in immune system disorders, allergies, and autoimmune diseases, often through research-driven approaches. In contrast, rheumatologists focus on musculoskeletal disorders, providing direct patient care and managing conditions like arthritis and lupus. Aspiring medical professionals should base their decisions on factors like personal interests, career aspirations, and job market outlook. By researching educational requirements, exploring clinical experiences, and assessing personal strengths, individuals can align their career paths with their passions and contribute to medicine.
Discover top-tier medical training at the American University of Antigua (AUA) College of Medicine. Learn more about our specialized programs and take the next step towards advancing your medical career.
FAQ
Which specialty requires more years of training: immunology or rheumatology?
Both specialties involve a similar structure of training, but are focused on different areas of specialization. Aspiring immunologists and rheumatologists need to earn a bachelor’s degree (4 years), complete medical school (4 years), undergo a residency program (3 years), and pursue a fellowship (2-3 years). In total, it takes approximately 13-14 years to become either an immunologist or a rheumatologist.
Is it possible to switch careers from immunologist to rheumatologist?
It is possible to switch careers from immunology to rheumatology through additional training. An immunologist would need to complete a residency in internal medicine or pediatrics, if they haven’t done so already, followed by a fellowship in rheumatology to become a rheumatologist.
✅ Request information on AUA's MD program TODAY!